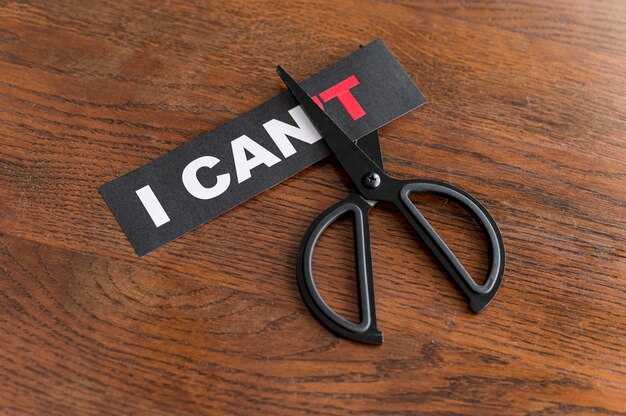
Would you be prepared to pose this question to your partner: when was the last time you felt lonely in this relationship? From what I observe, one person usually has no trouble bringing this up, while the other either never considers it or actively resists asking. If you’re the one who pulls back, pause and consider what runs through your mind when the idea of asking comes up. Do you fear being blamed, as if they’ll hold you responsible for their emotions? Are you afraid of losing your sense of independence — worried that probing into vulnerability will pull you into an unhealthy fusion where you no longer feel like yourself? Perhaps you feel ashamed, imagining they’ll use your inquiry as proof you’re failing, another reason to criticize how you fall short. Why would we intentionally open ourselves up to vulnerability if we expect it will only invite attacks or spark a fight? Those reactions are understandable, yet avoidance doesn’t resolve the underlying issue. The other person may already feel lonely in the relationship — do we honestly believe that ignoring it will make it vanish? Pretending everything’s fine and hoping distance will heal itself is a risky gamble. Left unaddressed, the distance and disconnection usually deepen. This isn’t about labeling you as the problem; rather, it’s about recognizing that assuming you’re at fault and dismissing their concerns only amplifies the dysfunction. In the end, ignoring or invalidating their feelings leaves them feeling more unheard, less loved, and less safe than before. The dismissiveness we justify as protecting the relationship often becomes the very thing that drives them away. So here’s straightforward advice: don’t let fear, shame, or assumptions steal from the partnership you want. Ask the difficult questions. If any of the fears I mentioned resonate with you, talk about them openly. Be transparent about how each of you experiences these issues. That kind of honesty is what actually builds intimacy and trust.
Practical steps to open the conversation
- Choose a calm moment with minimal distractions — avoid bringing this up during an argument or when either of you is rushed or exhausted.
- Use “I” statements to lower defensiveness: for example, “I’ve been feeling disconnected lately and I’m worried about loneliness between us. Can we talk about it?”
- Be specific and concrete. Point to recent moments (e.g., “Last week when you left the room while I was sharing, I felt dismissed”) rather than general accusations.
- Invite their perspective: “How do you experience our connection right now?” This signals curiosity rather than blame.
How to listen so the other person feels heard
- Reflect back what you heard before responding: “So you felt lonely when…” This validates their experience and clarifies misunderstandings.
- Ask open questions: “Can you tell me more about when that happens?” instead of yes/no questions.
- Avoid immediate problem-solving or defensiveness. Validation doesn’t mean agreement — it means acknowledging their feelings as real.
- Pay attention to nonverbal signals: tone, body language, and pauses often carry as much meaning as words.
What to avoid saying
- “It’s all in your head” or “You’re overreacting” — dismissive phrases shut down dialogue.
- Comparisons to other relationships or past partners — they minimize the current person’s experience.
- Instant retaliation or counter-accusations — if you feel attacked, request a pause and return to the topic when calmer.
Setting healthy boundaries and expectations
- Define what connection looks like for each of you: frequency of check-ins, quality time, physical affection, and emotional availability.
- Agree on small, achievable experiments (e.g., one uninterrupted 20-minute conversation each week) and revisit how they’re working.
- Respect autonomy: intimacy grows when both partners feel safe to be themselves, not when one is forced into constant closeness.
When loneliness stems from toxic patterns
- Notice recurring patterns: stonewalling, constant criticism, emotional unavailability, or manipulative behaviors. These are not solvable by one-sided effort alone.
- If one partner consistently invalidates feelings or retaliates for honesty, that is a sign the relationship may be harmful rather than merely troubled.
- Documenting patterns and setting clear consequences (e.g., “If we can’t discuss this without yelling, I will suggest a break or we’ll seek professional help”) can protect both partners’ emotional safety.
When to seek outside help
- Consider couples therapy if both of you are willing to work on the relationship but get stuck repeating the same fights or withdrawals.
- Individual therapy can help if you struggle with boundaries, fear of intimacy, or patterns that repeat across relationships.
- If either partner feels unsafe, threatened, or controlled, seek immediate support — hotlines, shelters, or trusted friends/family can help with a safety plan.
Self-care and support while you navigate this
- Maintain friendships and activities outside the relationship so you have perspective and emotional resources.
- Practice grounding and emotion-regulation techniques (deep breathing, short walks, journaling) before and after tough conversations.
- Be honest with yourself about what you can tolerate and what crosses a line. Protecting your own mental health is not selfish — it’s necessary.
Final note: asking “Are you feeling lonely?” is not a guarantee you’ll fix everything, but it’s the first step toward reversing isolation. Even if the answer is painful, honest curiosity and consistent follow-through create the conditions for real connection — or for a clear-eyed decision that the relationship isn’t meeting your needs. Either outcome is preferable to silent erosion.
Finding Healing: Steps to Rebuild Connection and Self-Worth

Set immediate safety and enforceable boundaries. List three non-negotiable limits (examples: no yelling, no monitoring phone, no unwanted visits). Write short scripts to use when a boundary is crossed (“If you raise your voice, I will leave the room.”) and practice them out loud three times. Track each boundary breach in a simple log for two weeks to spot patterns and decide next actions.
Create a safety plan with clear actions. Prepare a packed bag with ID, medication, cash, charger, and one change of clothes; store it in an agreed hideaway or with a trusted friend. Share a safe-word with one contact and set up a check-in schedule: daily text for two weeks after a heated interaction, weekly check-ins thereafter.
Book a therapy consult within 14 days. Choose a clinician experienced with relationship trauma or abuse and ask about CBT or EMDR in the first session. Use a weekly symptom rating (0–10) for anxiety, shame and trust; review scores each session to measure progress. If therapy waitlists are long, join an 8–12 week group with a trauma-informed facilitator.
Rebuild self-worth with a 6-week evidence plan. Each evening list three concrete accomplishments (no matter how small). Create a “strengths file” with 10 specific examples of when you solved problems or helped others; add one item weekly. Use mirror statements twice daily: short, factual phrases such as “I deserve calm” or “My choices matter.”
Use a structured thought record daily. For one trigger per day, note: situation, emotion (0–10), automatic thought, evidence for and against that thought, alternative balanced thought, and one small corrective action. Limit entries to 10–15 minutes to keep practice sustainable.
Practice grounding and breath work when triggered. Do a single 4-4-4 box breathing set (inhale 4s, hold 4s, exhale 4s) for two minutes, then a five-sense grounding check (name 5 things you see, 4 you can touch, 3 you hear, 2 you smell, 1 you taste). Repeat up to three times during a high-arousal episode.
Rebuild social ties with a low-risk plan. Identify two safe people and schedule one 30–60 minute contact per week (call, walk, coffee). Join a targeted community: a 6-week support group, a class related to an interest, or volunteer once a month. Track each social contact and rate comfort 0–10 to plan gradual increases.
Set small, measurable daily routines for body and mind. Aim for 20–30 minutes of movement three times weekly, 7–9 hours of sleep per night, and reduce alcohol or substances by 50% over four weeks if they fuel isolation. Add a five-minute morning ritual: hydration, one goal for the day, and one sentence of gratitude.
Repair communication skills with targeted practice. Use “I” statements and short requests: “I feel upset when X; I need Y for now.” Role-play these lines twice weekly with a friend or therapist. Limit conflict discussions to 20 minutes and schedule follow-up only if both parties agree to stay calm.
Monitor progress with weekly checkpoints. Every Sunday, review your boundary log, symptom ratings, therapy notes, and social contact tracker. Adjust one specific behavior for the next week (for example, add a second safety check-in, extend therapy homework, or increase social contact by one call).
Address setbacks with a concrete reset plan. If a boundary is broken or trust is violated, pause contact for a defined period (24–72 hours), notify your support person, and follow a three-step reset: review the event, complete two calming practices, and decide one measurable next step (e.g., change living arrangements, increase therapy frequency).
Use these steps consistently for four to twelve weeks and adapt based on measurable changes in safety, mood ratings and relationships.


 Toxic Relationships are Lonely!">
Toxic Relationships are Lonely!">

 Relationship EXPERT reveals Secrets to Connection: Dr. Sue Johnson">
Relationship EXPERT reveals Secrets to Connection: Dr. Sue Johnson">
 Чи вас оточують хулігани? Прихована причина, чому ви їх пускаєте.">
Чи вас оточують хулігани? Прихована причина, чому ви їх пускаєте.">
 Поведінка вашого партнера пов’язана з травмою, але це все одно не нормально.">
Поведінка вашого партнера пов’язана з травмою, але це все одно не нормально.">
 Найсильніший Ознака того, що Уникаючий Все Ще Глибоко Вас Кохає">
Найсильніший Ознака того, що Уникаючий Все Ще Глибоко Вас Кохає">
 Якщо Ви Вимикаєтеся Під Час Конфлікту, Подивіться Це">
Якщо Ви Вимикаєтеся Під Час Конфлікту, Подивіться Це">
 If Your Partner Says These Phrases, They’re an Avoidant">
If Your Partner Says These Phrases, They’re an Avoidant">
 Until This One Shift Finally Made the Avoidant Come Back | Mel Robbins Motivational Speech">
Until This One Shift Finally Made the Avoidant Come Back | Mel Robbins Motivational Speech">
 For Healing, Sane Action is More Powerful Than Sad Stories">
For Healing, Sane Action is More Powerful Than Sad Stories">
 A Partner Needs to Know About Your Past — But What If You’re Just Dating?">
A Partner Needs to Know About Your Past — But What If You’re Just Dating?">
 CHEATING is for SELFISH COWARDS (like me)">
CHEATING is for SELFISH COWARDS (like me)">