Schedule a daily 10-minute breathing checkpoint immediately upon waking: perform 4-count inhale, 6-count exhale, repeat 6 cycles; record three observations via writing: bodily sensations, clear triggers, one tiny action to take that day. This precise micro-routine boosts calm, helps center attention, aids managing intrusive thoughts, and improves getting control during high-demand moments.
Create 10-item lists of micro-commitments to rebuild a stable foundation: sleep target 7–8 hours, caffeine cutoff at 14:00, 30-minute brisk walk five days weekly, two 20-minute creative sessions weekly. Schedule small pleasures twice weekly as soul-filled appointments; mark them as planned in a calendar and treat removal of one habit as an experiment in balance. Track which causes of unease recur, then redesign the next week with different corrective actions.
Practice separating work identity from private life through concrete boundaries: power down laptop at a set hour, route notifications to Do Not Disturb at night, create a physical center in the home that’s tech-free. Use a bedside brain-dump of thoughts–five minutes of rapid writing–to offload rumination, making it easier to fall asleep and reduce reactive behavior the next day.
Convert intentions into measurable metrics: log calm-days per week, count completed planned pleasures, note nights with uninterrupted sleep. Aim to increase calm-days by roughly 20% within eight weeks; if progress stalls, change one habit at a time. Consider brief consultations with a clinician or peer coach; anecdotal guidance from scott and others highlights that small, consistent adjustments compound into lasting balance.
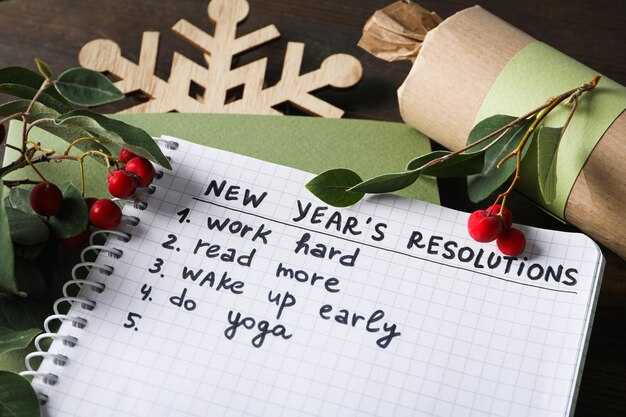
Practical plan: 10 resolutions paired with a 5-step routine
Begin mornings: 10-minute diaphragmatic breathing; 30-minute brisk walk; 5-minute prioritized task list to manage energy and reduce spike in cortisol.
| 약속 | Step 1: Plan | Step 2: Prepare | Step 3: Execute | Step 4: Measure | Step 5: Adjust |
|---|---|---|---|---|---|
| Daily movement | 30 min brisk walk, target 5x weekly | lay out shoes, route, weather check | walk at 4–6 km/h, log duration | track steps; expect reductions in sedentary time ~40% | increase intensity 5% weekly until sustainable |
| Consistent sleep window | 7–8 h nightly, fixed wake time | set alarm, dim lights 60 min before | sleep at same clock time, no screens | collect sleep hours; cohort data links consistency to lower obesity incidence | shift 15 min earlier each week until stable |
| Strength training | 3 sessions weekly, 20–30 min | setup weights or resistance band | compound moves: squats, presses, rows | log reps; expect muscle maintenance that raises basal metabolic rate | add 2–3 reps per set weekly |
| Digital curfew | no screens 60 min before bed | place phone in another room | read, stretch, light breathing | measure sleep latency; typical reductions ~20% in trial data | move curfew 10 min earlier weekly until target met |
| Music reset | 15 min of slow ballad or calm tunes | create playlist labeled “soul-filled reset” | listen during transition breaks | monitor heart rate; short sessions lower rate around 5–10 bpm | swap tracks that doesnt lower baseline heart rate |
| Microbreaks | 5 min break every 50 min work | timer app set to 50/5 cycle | stand, stretch, hydrate | measure output; typical productivity gains ~10–25% | adjust timing to match peak focus periods |
| Hydration target | 2 L plain water daily | fill bottle before leaving desk | sip steadily, avoid sugary drinks | note urine color; keeps bodys fluid balance optimal | add electrolyte if long sweat sessions occur |
| Declutter transitions | 10-min ritual between work and home | close laptop, change clothes, short walk outside | apply ritual to separate roles | survey perceived boundary quality; separating spaces opens clearer focus | refine ritual until transition feels easier |
| Social touchpoints | 2 meaningful contacts weekly | schedule calls, coffee, or walk | engage with direct questions, listen | track mood scores; social data shows modest boosts in wellbeing | prioritize connections that add warmth and sustain energy |
| Evening reflection | 2-minute gratitude or micro-journal | keep pen and small notebook bedside | write 3 short items: done, learned, next | score nightly mood; small shifts move baseline forward | update prompts that dont yield clarity |
Five-step routine applied across these commitments: plan with certain metrics and target dates; prepare equipment or environment to enter activity quickly; execute with timed intervals and simple cues; measure small data points daily to understand progress; adjust cadence to manage adherence and sustain reductions in unwanted symptoms. Use a leader habit each week that opens access to other commitments; here a single effective cue makes cascading changes easier. If a commitment doesnt fit schedule, split activities into 10–15 minute units around peak energy periods. Always log one metric per commitment; below that log, add qualitative notes about warmth, mood and energy. These concrete measures let you understand trends, protect bodys resources, reduce risk markers such as obesity, and push productivity forward.
Resolution 1 & 2: Daily 5-Minute Deep Breathing and 10-Minute Structured Breaks
Practice 5 minutes of diaphragmatic breathing twice daily: inhale 4 seconds, hold 4 seconds, exhale 8 seconds; complete 8–10 cycles to target 6–8 breaths per minute; expect a typical resting heart-rate reduction of ~3–10 bpm and measurable increase in heart-rate variability within 2–4 weeks – an effective, low-effort routine.
Sit upright with neutral spine, shoulders relaxed; place one hand on chest and one on abdomen where abdominal expansion is felt; breathe through the nose, letting the abdomen rise while the chest moves less; center attention around tactile sensations and lengthen the exhale to bias a parasympathetic response; relax jaw, neck and shoulder muscles.
If breathing practice provokes reactive sensations or panic, switch to box breathing (4-4-4-4) or start with 2-minute sets, increasing duration by 1 minute every 3 days; track baseline resting heart rate plus perceived arousal on a 1–10 scale; consult a qualified therapist when conflicted about symptoms such as persistent dizziness, chest discomfort, or escalating anxiety.
Schedule a 10-minute structured break every 50–90 minutes of focused work: set a timer, stand and walk 100–150 steps, perform three mobility moves targeting hips, shoulders and lower back (hold each 15–30 seconds), drink 150–250 ml water, then include 2 minutes of breathing practice to recharge cognitive control and reduce midday fatigue.
Contents of an optimal break: 2 minutes mobility, 3 minutes sensory reset (short outdoor exposure or window view), 3 minutes low-intensity movement, 2 minutes planning the next work block; use musicis set at 60–70 BPM during the sensory reset as a relaxing anchor; avoid screens when negative rumination tends to increase.
Adherence tactics: add short breathing sessions as calendar events, pair break timing with hydration and brief nutrition, use phone alerts labeled ‘Breathe’ and ‘Break’ making sustained practice easier; small daily effort delivers huge cumulative gains, strengthening attention and stamina throughout successive workdays and raising long-term resilience.
Safety notes: avoid prolonged rapid breathing due to risk of dizziness and tingling; always stop if chest pain or severe lightheadedness appears and seek medical evaluation; this approach is helpful when reactive to fight-or-flight triggers and may require therapist guidance when trauma history exists.
Resolution 3 & 4: Short Morning Movement and a Consistent Bedtime Window
Do a 6-minute morning mobility circuit immediately after waking: 60s joint circles and shoulder rolls, 90s hip hinges + glute bridges, 90s slow bodyweight squats + calf raises, 60s single-leg balance, 60s diaphragmatic breathing at a 4-4-6 cadence; perceived exertion 5–7/10, heart rate <60% max.
- Contents of the circuit: gentle joint work to enter movement without jolting the brain, dynamic stretches to reduce a cluttered morning mind, and a final breath set that feels relaxing and grounding.
- Progression: add 10–20s per block every week until the full set reaches 10–12 minutes, or swap one block for a 45s plank once strength improves.
- Daily timing: complete within 15 minutes of waking and at least 60 minutes before intense cognitive work to let the brain shift from fight-or-flight to a grounded state.
- Practical metric: if balance holds 45s single-leg without wobble, increase squat depth or add a controlled tempo to keep adaptations moving further.
- Goal alignment: doing this sequence five times per week creates an excellent baseline habit that will reduce morning agitation and improve ability to face long work blocks.
Bedtime window protocol (pick one 30–60 minute anchor that matches your schedule):
- Set a fixed sleep-onset window (example: 22:30–23:00). Keep wake time within ±30 minutes to stabilize circadian cues.
- 60–90 minutes before the window: dim lights, stop screens, perform a 10-15 minute separating ritual – quick worry list, one sentence of prioritization, then a relaxing physical routine or light reading.
- Limit caffeine and intense exercise so that sleep latency stays under 30 minutes; adults who reduce evening stimulants typically see sleep latency drop 10–20 minutes within two weeks.
- Use gentle breathing (4-4-6) or progressive muscle relaxation in the last 10 minutes; listening to a calm voice or white noise is acceptable if it helps you switch off.
- If sleep is repeatedly elusive after 30 minutes, get out of bed and do a low-stimulation activity until drowsy, then re-enter the window; avoid long naps that shift circadian phase.
- Quick metrics to track: time in bed, sleep-onset latency, wake-after-sleep-onset; aim for consistent wake time and 7–9 hours total sleep opportunity if you are adults with typical needs.
- Social tip: talk with friends about scheduling conflicts early; different household routines may require staggered windows but the path toward regular sleep remains the same – consistent cues.
- Mental health safety: if thoughts become overwhelming or suicidal, contact emergency services or a crisis line immediately; it is okay to ask for help and to tell someone you trust. An editorial note: persistent severe symptoms carry clinical risk and need urgent attention from a clinician.
- Behavioral boundary: separating worry from sleep means writing concerns down and deferring problem-solving until morning; this reduces cognitive load and stops the flight response from hijacking sleep.
- Long-term: following both the short morning routine and a steady bedtime window will shift homeostatic pressure and circadian rhythm, lowering nighttime arousal and improving daytime concentration within 2–6 weeks.
Checklist below (copy into a planner):
- Morning circuit entered within 15 minutes of waking – duration: 6–12 minutes.
- Fixed bedtime window set and practiced ≥5 nights weekly.
- Pre-bed separating ritual completed 60–90 minutes before sleep-onset window.
- Track core metrics weekly and adjust light exposure, meal timing, caffeine timing, and exercise timing if sleep shifts from target.
- If uncertain what will help next, talk to a clinician or sleep coach; listening to professional guidance is an excellent step away from trial-and-error.
Resolution 5 & 6: Mindful Eating Cues and Limiting Stimulants After Noon
Rate hunger 1–10 before you enter the kitchen; if the score is below 4, wait 20 minutes, drink 250 ml water and reassess. Get others involved by using a one-line pre-meal checklist that records what you will eat, why you chose it and an expected satiety score – this planned step opens a clear direction and helps you stick to portions. Take 3 slow diaphragmatic breaths immediately prior to the first bite, chew each mouthful 20–30 times, pause every 5 minutes to note a single thought about how you feel, and stop when satiety drops by 2 points from the pre-meal rating. Use plate targets: hand-sized protein, fist-sized carbohydrate, two cupped handfuls of vegetables; reducing plate diameter by 20% typically reduces intake without increasing hunger. A no-screen policy at the table keeps attention on the moment and reduces unplanned spending of calories by an estimated 10–20%. Professional therapists’ advice: log three meals per week with timestamps and one-line notes about mood; 4 weeks of consistent logging establishes habit direction.
Stop caffeine intake at 12:00; cap total daily caffeine under 300 mg and prefer decaf, herbal tea or water while having mid-afternoon tasks. Caffeine half-life averages 5–6 hours: 200 mg at 12:00 leaves ~100 mg at 17:00 and ~50 mg at 22:00, which can affect sleep onset and cause measurable productivity loss next day in the workplace. Replace an afternoon espresso with a 10–15 minute brisk walk, a 15-minute power nap (keep nap <20 minutes), or low-volume tunes at 60–80 bpm to slow eating pace and reset alertness. a simple office beverage policy – label mg per cup, stock decaf options, schedule coffee breaks before noon reduces late stimulant exposure opens alternatives that minimize sleep loss. track response: if latency increases>15 minutes or daytime tiredness rises while reducing caffeine, lower late intake further and consult a clinician or therapist.
Resolution 7 & 8: Time-Blocking Worry Time and Digital Detox Evenings
Schedule a fixed 20-minute “worry slot” daily (example: 18:30); set a physical timer, list each worry on one line, assign a 0–10 intensity rating before and after, and pick a single actionable next step per worry to execute later; outside that window defer intrusive thoughts by jotting them into a dedicated notebook and postponing engagement until the slot. Measure baseline intensity three days prior, track daily scores, calculate weekly mean and aim to reduce that mean by 2 points over four weeks. If GAD-7 ≥10 or symptoms persist 14+ days, seek counseling – adults with recurrent panic, sleep loss, or functional impairment should contact a clinician (источник: GAD-7 guidance). This protocol moves reactive rumination into scheduled, problem-solving time and will shape calmer habits that reduce feeling overwhelmed, help mentally reorganize priorities, and allow gradual growth away from past patterns of constant reactivity.
Adopt a 90-minute evening screen cutoff: power down phones and tablets at 21:00, enable airplane mode or Do Not Disturb, and switch to printed reading, light stretching or low-intensity sports and play (walking, gentle yoga) earlier in the wind-down period. Use phone screen-time stats to measure reduction in nightly usage and record sleep onset latency and total sleep hours nightly; target a 15–30 minute drop in latency within two weeks, and further improvement thereafter. On particularly challenging or stressful days simply shorten the worry slot to 10 minutes rather than skip it; adjust tempoespecially of evening activity after intense workdays to remain calmer. Regularly review logged scores against past baseline to confirm measurable improvement; if improvements stall, consider brief counseling sessions as a next step.
Resolution 9 & 10: Social Support Check-ins and Self-Compassion Practices
Schedule two 15-minute social check-ins weekly with 1–2 trusted contacts plus a 10-minute nightly self-compassion meditation; measure mood and key symptoms on a 0–10 scale prior to each practice and again afterward.
-
Structure of social check-ins
- Start: 60 seconds naming current state (use single words: fine, anxious, overwhelmed, angry).
- Share one specific need: practical help, an active listener, or a short text reminder at night.
- End: two action steps and a precise time to follow up next session.
-
Scripts and micro-prompts
- “I’m having increased anxiety today; can you hold space for 10 minutes?”
- “If I seem negatively reactive, say ‘grounded?’ and wait two breaths.”
- Keep writing one-line logs after each check-in: date, mood score, trigger, action taken.
-
Measurement routine
- Daily quick log: mood (0–10), hours sleep, anger spikes count, anxiety symptom count.
- If anxiety or anger ratings increase by 2+ points across 3 days, escalate: contact your therapist within 48 hours or add an extra check-in the next day.
- Review trends every 30 days and compare direction from prior months and years to track progress.
-
Boundaries and limits
- Say “I need 24 hours to respond” when having heavy emotions; keep replies short until calmer.
- Limit vent sessions to one scheduled slot weekly; other times use micro-checks to stay grounded.
- If a confidant’s tone is negatively affecting sleep or mood, reduce frequency and explain the change.
Self-compassion practice plan with exact steps and timing to make coping easier and more balanced:
-
Nightly 10-minute routine
- Minute 0–1: Sit, place hand on chest, breathe slow.
- Minute 1–4: Body scan, name sensations without judgement.
- Minute 4–8: Compassion phrases aloud three times each: “May I be safe,” “May I be kind to myself,” “May I allow rest.”
- Minute 8–10: Visualize one small step to move forward tomorrow; set that single intention.
-
Two-minute on-demand scripts
- When anger rises: label “anger” once, exhale slowly five times, press feet to ground to feel grounded.
- When anxious or overwhelmed: name the top symptom, rate it, then say a short compassion line aloud.
- Use a 5-4-3-2-1 sensory check to shift out of spirals.
-
Writing prompts that are actionable
- Evening: “Today I felt X; one cause was Y; one small step that helped was Z.”
- Weekly: “Which interactions increased anxiety or helped me feel better?” Mark patterns and adjust social plan accordingly.
-
When a child is involved
- If parenting duties leave you overwhelmed, schedule a 10-minute check-in during a nap or quiet time and ask one household member to take one task each week.
- Teach a short box-breathing routine to older children so shared breathing reduces household tension and anger spillover.
-
Progress metrics and clinical triggers
- Track symptom direction weekly; aim at a net decrease in anxiety score over 8–12 weeks while keeping activity balanced.
- Contact a therapist when symptoms increase rapidly, sleep drops below 5 hours three nights in a row, or coping feels ineffective despite scheduled practices.
- Expect steady shifts across months and years; small, consistent actions make change easier and help keep you grounded.
Quick checklist to implement now: pick two contacts, add two 15-minute slots to calendar, set a nightly alarm for the 10-minute meditation, begin a one-line writing log tonight, and remeasure mood in seven days to see early direction.
5-Step Daily Routine to Try: Step 1 – Breath to Start, Step 2 – Gentle Movement, Step 3 – Mindful Moment, Step 4 – Screen-Free Wind-Down, Step 5 – End with Reflection

Step 1 – Breath to Start: Do 6-4-6 box breathing: inhale 6s, hold 4s, exhale 6s; repeat 6 cycles (≈5 minutes). Place one hand on chest, one on abdomen to feel diaphragm; sit upright, eyes closed. This activity raises heart rate variability when baseline is high and reduces amygdala reactivity, researchers report measurable drops in anxious and anger symptoms within 10 minutes. If heartbeat feels very high, shorten inhale to 4s and extend exhale to 8s. Gentle temple massage also calms the nervous system.
Step 2 – Gentle Movement: 10–20 minutes of low-impact activity such as slow walking or a short yoga sequence (cat-cow x10, child pose 2 minutes, standing forward fold 5 breaths); pace should remain conversational. Such movement improves sleep hours and reduces restless brain activity in the long term, with small studies showing better mood across a year when practiced regularly. If pain limits access to movement, consult a physical or mental-health professional to receive alternative options and precise advice.
Step 3 – Mindful Moment: Sit 5 minutes and run a body scan; write three short notes about sensations, energy and triggers, then review them. This practice identifies aspects that tend to escalate sadness, anger or anxious rumination, which helps plan coping moves. If writing stirs suicidal thoughts or severe symptoms, visit emergency services or a clinician immediately; talking with a trusted other usually reduces isolation and can help access urgent support quickly. Include a soul-filled sentence of gratitude to balance intense material.
Step 4 – Screen-Free Wind-Down: Cease screens 60–90 minutes before bedtime; choose a low-arousal activity like reading print, light stretching, a warm shower or tea to introduce physical warmth and prepare the brain to enter sleep in a calm state. Blue light negatively shifts melatonin timing and can increase evening anxious feelings and worst-case sleep fragmentation; shut devices outside the bedroom to limit access and reduce expectancy of late alerts. If partners are talking nearby, set a brief window to finish conversations early so both can enter rest mode.
Step 5 – End with Reflection: Spend 5–10 minutes writing a micro-review: list three wins, one trigger that made you feel angry or anxious, and one small coping action to try the next morning. Note where symptoms spike during the day and mark lifestyle adjustments that reduce negative patterns. Set a clear intention to enter sleep with calm imagery and high expectancy about tomorrow; those who keep this short practice show improved mood in clinical reviews. If suicidal thoughts persist or worst symptoms escalate, visit crisis services immediately and seek a trained professional.


 10 새해 결심으로 스트레스 해소하기">
10 새해 결심으로 스트레스 해소하기">

 감정적 스트레스 인식 및 대처 방법 – 더 나은 정신 건강을 위한 실용적인 전략">
감정적 스트레스 인식 및 대처 방법 – 더 나은 정신 건강을 위한 실용적인 전략">
 4 이혼의 예측 요인 및 대처 방법 – 관계를 구하기 위한 실용적인 팁">
4 이혼의 예측 요인 및 대처 방법 – 관계를 구하기 위한 실용적인 팁">
 5 Essential Components of Emotional Intelligence to Lead More Effectively">
5 Essential Components of Emotional Intelligence to Lead More Effectively">
 15 Signs of Passive-Aggressive Behavior With Examples – How to Recognize and Respond">
15 Signs of Passive-Aggressive Behavior With Examples – How to Recognize and Respond">
 네, 당신은 안전하게 이기적인 사람을 떠날 수 있습니다. 안전하게 빠져나와 자신을 보호하는 방법은 다음과 같습니다.">
네, 당신은 안전하게 이기적인 사람을 떠날 수 있습니다. 안전하게 빠져나와 자신을 보호하는 방법은 다음과 같습니다.">
 혹시 식사하셨나요? 음식은 최고의 아시아식 애정 표현입니다.">
혹시 식사하셨나요? 음식은 최고의 아시아식 애정 표현입니다.">
 자기 계발 중독될 수 있을까요? 징후, 위험, 그리고 건강한 성장">
자기 계발 중독될 수 있을까요? 징후, 위험, 그리고 건강한 성장">
 지연을 멈추는 방법: 2분 규칙 – 지금 바로 시작하기 위한 빠르고 실용적인 가이드">
지연을 멈추는 방법: 2분 규칙 – 지금 바로 시작하기 위한 빠르고 실용적인 가이드">
 자신에게 삶을 살아갈 수 있는 허락을 주세요 – 프리야 라나 카푸르">
자신에게 삶을 살아갈 수 있는 허락을 주세요 – 프리야 라나 카푸르">
 질투심 vs. 시샘 – 차이가 있을까요? 명확한 가이드">
질투심 vs. 시샘 – 차이가 있을까요? 명확한 가이드">