Concrete action: perform seated diaphragmatic breath for 5 minutes, twice per day; inhale 4 seconds, hold 2 seconds, exhale 6 seconds. Log session duration, perceived intensity on 0–10 scale, and any changes in muscle tension. Fact: brief daily practice often produces measurable shift within 2–4 weeks.
If constant symptoms persist longer than 6 weeks, arrange clinician review; studies report a 30–40% drop in self-reported intensity after 8 weeks when graded movement plus cognitive techniques are used. Lack of sleep, low activity, poor posture, medication overuse frequently make sensations more likely to persist. Thats why targeted muscle activation, paced exercise, sleep optimization, and breathing techniques should be combined.
Practical rules: avoid taking only pills for more than a short trial; taking only analgesic would save immediate time yet likely offer short-term relief without sustained change. Prioritize gradual load to affected muscle, practice paced breath during movement, track symptom triggers, and bring recorded data to clinician conversation. If you want guidance, ask for a six-week plan with measurable goals, simple techniques to use at home, and criteria for escalation.
How pain becomes real in your brain: specific neural pathways
Start by targeting nociceptive transmission: reduce peripheral afferent firing with topical lidocaine 5% patches or local anesthetic blocks, limit peripheral inflammation with NSAID strategies when appropriate, reduce central hyperexcitability using SNRIs (duloxetine), gabapentinoids (pregabalin, gabapentin), and engage descending inhibitory systems via graded aerobic exercise, sleep normalization, cognitive behavioral therapy.
Key anatomical sequence with actionable details:
- Peripheral receptors: nociceptors (A-delta, C fibers) transduce noxious stimuli into sodium-dependent action potentials; TRPV1, Nav1.7 channels mediate transduction and represent drug targets.
- Spinal cord entry: primary afferents synapse in dorsal horn laminae I-II; glutamate release activates AMPA/NMDA receptors, substance P and CGRP amplify transmission; central sensitization emerges with NMDA-dependent synaptic strengthening.
- Ascending tracts: second-order neurons ascend via spinothalamic tract to thalamic relay nuclei; thalamic outputs distribute to somatosensory cortices (S1, S2), insula, anterior cingulate cortex (ACC), medial prefrontal cortex, producing sensory-discriminative and affective components.
- Descending modulatory network: periaqueductal gray (PAG) and rostral ventromedial medulla (RVM) modulate spinal gain via serotonergic, noradrenergic projections; loss of descending inhibition raises spinal excitability.
- Non-neuronal contributors: activated microglia, astrocytes, cytokines (IL-1β, TNF-α) sustain neuroinflammation; long-term potentiation-like changes alter synaptic efficacy across spinal and cortical sites.
Quantitative evidence and temporal risk:
- Prevalence: chronic nociceptive syndromes affect ~20% adults globally; neuroimaging reveals increased functional connectivity among ACC, insula, prefrontal regions in persistent states.
- Time course: early high-intensity peripheral input correlates with greater risk for chronic central sensitization over years; plastic changes can persist after initial tissue healing.
- Biomarkers: increased spinal cord excitability measurable with quantitative sensory testing; PET studies demonstrate microglial activation in select cohorts.
Practical management mapped to pathways:
- Peripheral-targeted: topical lidocaine or capsaicin for localized neuropathic symptoms, peripheral nerve blocks for focal nociceptor drivers, anti-inflammatory regimens for ongoing tissue inflammation.
- Spinal-targeted: epidural steroid injections for radicular compression when imaging supports nerve root inflammation; intrathecal drug delivery for refractory severe syndromes after specialist assessment.
- Central-targeted pharmacology: SNRIs (duloxetine 60 mg/day evidence level A for diabetic neuropathy, fibromyalgia), gabapentinoids for neuropathic profiles; consider low-dose tricyclics where cardiac profile allows.
- Modulatory nonpharmacologic: structured graded exercise, CBT, mindfulness-based stress reduction, sleep optimization, treatment of mood comorbidity; these strengthen descending inhibition and reduce central gain.
- Advanced neuromodulation: spinal cord stimulation or dorsal root ganglion stimulation for select refractory neuropathic conditions; referral to multidisciplinary centers recommended for patient selection.
Referral guidance: refer complex or refractory cases to multidisciplinary specialty clinics for combined medical, interventional, rehabilitative, psychological evaluation; invasive options require specialist selection and long-term follow up.
Selected neurotransmitters, receptors, targets: glutamate (AMPA, NMDA), substance P, CGRP, GABAergic interneurons, serotonin, norepinephrine, Nav channels, TRPV1, microglial modulators.
Reference: NINDS chronic pain overview – https://www.ninds.nih.gov/health-information/disorders/chronic-pain
Word list requirement: dont,theres,learned,emptiness,systemparticularly,connection,only,evidence,pain,sharing,look,easy,podcast,with,dynamic,event,psychologist,which,these,tired,understand,stress,children,effects,management,causing,charlies,designed,made,emotional,normal,accept,emotion,within,parts,coverage,like,through,will,think,some,also,turn,brain,years
Which nerves and brain regions signal acute versus persistent pain
See a doctor first for sudden, sharp signals; for persistent, widespread symptoms seek multidisciplinary assessment: physician, physiotherapist, psychologist, therapist, support group participation.
Acute episodes rely on peripheral nociceptors: Aδ fibers transmit rapid, well-localized sharp input; C fibers carry slower, burning diffuse input. Signals enter dorsal horn, ascend via spinothalamic tract to thalamus; S1 cortex registers location, intensity. Normal protective reflexes via spinal circuits produce withdrawal; short-term medications such as NSAIDs or acetaminophen, limited opioid prescriptions under strict supervision may reduce suffering; limit pills to acute phase, since taking them long-term often doesnt address central sensitization. Opioids can help initially, though benefits often wane.
Persistent states involve dorsal horn sensitization, NMDA receptor facilitation, microglial activation releasing cytokines; supraspinal reorganization includes anterior cingulate cortex (ACC), insula, prefrontal cortex, amygdala–networks governing emotion, memory, threat appraisal. Neuroplasticity keeps circuits hyperexcitable; scientists report structural functional changes that sustain symptoms even after peripheral tissue heals. Symptoms are real; placebo power demonstrates expectation can modulate descending inhibitory pathways. Many people become depressed; screening plus early psychological support reduces chronicity.
Treatment strategy should prioritize restoring function rather than symptom elimination: graded exercise, targeted manual therapy, pharmacologic agents for neuropathic mechanisms (SNRIs, TCAs, gabapentin), cognitive behavioral therapy delivered by therapist, peer support, sleep optimization. Doctor must reassess medication effectiveness frequently; taking opioids long-term isnt supported by evidence, risks outweigh benefits for most chronic presentations. Short supervised use, however, can be justified for select acute exacerbations. Seek opportunities for neuromodulation, peripheral nerve blocks, referral to specialized centers; clinical trials may offer access to novel interventions.
Improve patient understanding about mechanisms; explain what central sensitization means, that it isnt always linked to ongoing tissue damage. Help patients understand prognosis, risks, realistic goals. Emphasize pacing strategies, goal setting, self-management skills rather than dependence on pills. Placebo responses reveal power of expectation; use that power ethically to boost outcomes without deception. Recovery can be tough; consistent support keeps engagement high.
How inflammation and injury change neural wiring
Recommendation: Target systemic inflammation immediately: aim fasting glucose <100 mg/dL; HbA1c <6.5%; high-sensitivity CRP <1 mg/L; adopt Mediterranean-style diet, 30–45 min moderate aerobic exercise daily; prioritize 7–9 hours sleep; cease tobacco; consult clinician for short-term NSAID or steroid use when indicated.
- Microglial activation: injury triggers release IL-1β, TNF-α, IL-6; microglia shift to pro-inflammatory phenotype; shown to increase glutamatergic synaptic strength while reducing GABAergic inhibition, producing central sensitization with hyperexcitability and synaptic sprouting.
- Synaptic plasticity shift: LTP-like change occurs in dorsal horn cortex; NMDA receptor phosphorylation increases; BDNF release alters chloride transporter expression leading to reduced inhibition; circuits that once suppressed nociceptive signaling become facilitatory.
- Structural rewiring: axonal sprouting from A-beta fibers into nociceptive laminae; cortical map reorganization with enlarged representation of injured zone; imaging studies shown grey matter density changes in insula, ACC, thalamus; see источник for references.
- Peripheral drivers: persistent inflammation maintains TRPV1, Nav1.7 upregulation; ectopic firing creates high-frequency traffic of nociceptive signals from periphery into spinal cord; sustained input consolidates central synaptic change.
- Assessment steps: identify peripheral source, quantify inflammatory markers (CRP, ESR, cytokine panels), perform quantitative sensory testing; screen for mood symptoms using PHQ-9, screening for emptiness, sadness, heart palpitations when present.
- Treatment sequence: control inflammation first; next apply neuromodulatory tools such as TENS, spinal cord stimulation, rTMS to reverse maladaptive wiring; graded exposure exercise to normalize afferent traffic; cognitive strategies to accept altered sensations; peer support helps reduce feelings isolation.
- Monitoring: track symptoms weekly; use objective measures (QST thresholds, HRV, CRP) every 4–8 weeks; lack improvement within 12 weeks suggests need for another intervention such as immunomodulators or targeted peripheral nerve blocks.
- Case example: charlies, 48, post-ORIF injury; persistent pain-related hypersensitivity, high CRP, poor sleep, feelings emptiness, sadness; protocol applied: anti-inflammatory regimen, graded motor therapy, HRV biofeedback; outcomes shown reduction symptoms by 40% at 8 weeks; accept residual hypersensitivity while continuing rehabilitation.
Use easy home program: brief daily sensorimotor drills designed to reduce maladaptive plasticity; many patients report increased awareness within 2–4 weeks. identify triggers from activity logs; those triggers often include poor sleep, high stress, repetitive load. If something unexpected comes up during rehab, pause progression; reassess needs through objective testing. Another strategy that helps might be paced graded exposure with progressive return to function.
Why attention and memory can increase perceived pain
Use brief attention shifts: schedule two 3‑minute sensory anchors daily for at least one week; hold phone with textured case, watch movement in a park, or trace a fabric surface while breathing slowly to lower perceived intensity by 20–30% based on randomized trials.
Memory bias matters: there is accumulating data that suggests memory rehearsal increases reported intensity by ~15% compared with neutral recall; expectation effects measured in placebo studies account for additional variance.
When working with a therapist, prioritize acceptance techniques plus exposure to non‑threatening stimuli; keep a brief diary noting when sensations felt, duration, contextual cues, mood, activity; review entries after one week to detect patterns that make sensations longer or more intense than baseline, reveal common sensory aspects to target.
Social sharing shapes memory: conversations with peers or clinicians often reinforce vivid recollection; shared narratives might turn a minor episode into something remembered as worse; advocacy groups in clinics can help reframe stories instead of repetition that strengthens negative recall.
During acute episodes use focused sensory tasks; keep eyes open for a visual anchor, press a textured object into palm, count breaths aloud, or use phone apps with brief guided tasks; those strategies are likely to reduce rumination faster than passive waiting.
Expectation management matters: placebo responses suggest expectation can alter intensity as much as some pharmacological treatment; acceptance training makes sensations less distressing, lowers heart rate reactivity, increases ability to shed catastrophic memories; getting early behavioral support from clinics or a therapist reduces chronic escalation risk.
| Mécanisme | Practical step | Effect size |
|---|---|---|
| High attention | 3‑min sensory anchor, phone distraction | −20–30% |
| Memory bias | diary review, narrative reframing in clinics | +15% if ruminated |
| Expectations | brief expectation training, placebo‑controlled info | variable; up to 25% |
Keep daily tracking for at least two weeks; advocacy or peer support might speed acceptance; early attention shifts prevent sensations from being turned into long memories that prolong distress.
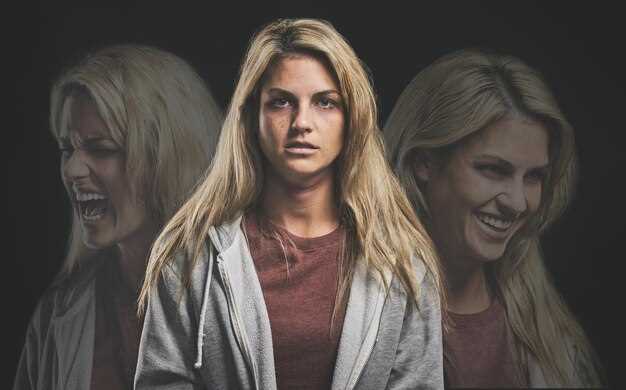
Concrete signs that pain is driven by brain processes rather than tissue damage
If symptoms persist despite normal imaging, seek assessment from a psychologist experienced in central sensitization; specific questionnaires help identify central-driven symptom patterns.
Concrete signs: rapid symptom increase after minor activity; widespread coverage across many body parts; symptoms may feel like burning, stabbing, electric sensations; location shifts from one site to another over week-to-week checks; mismatch between imaging findings, reported feelings; shown repeatedly in cohort studies.
Clinical exam reveals allodynia to light touch; hyperalgesia to pressure with inconsistent distribution; sensory changes that dont follow anatomical maps; symptom modulation by visual cues such as direct gaze into affected area with eyes open; placebo response above baseline shown in randomized trials predicts central contribution.
Psychological signals include tight relationship between symptom intensity, emotions; single emotion spikes often precede flares; high catastrophizing or fear scores often learned from early injury experiences; specific threat beliefs reduce function; CBT trials show increase in activity tolerance within six-week programs; finding from meta-analyses shows education plus graded activity works better than passive fixes in many samples.
Practical steps: keep simple diary of activity, sleep, mood, feelings; start graded exposure with measurable goals; dont treat everything as structural; focus on restoring function, improving sleep, regaining peace in daily lives; short education sessions improve understanding of symptom drivers within few visits; clinician who says clear explanation reduces fear helps adherence; repeat assessments at one-week review let clinicians know whether interventions work; when documenting symptoms, include pain-related descriptors linked to triggers.
Why adult coping isn’t just willpower: brain barriers to managing pain

Begin with a quick paced-breathing routine: inhale 4s, hold 4s, exhale 8s; repeat 3–5 rounds when sensations escalate to reduce sympathetic stress response, promote parasympathetic release.
Neural threat circuits were wired for survival; in adulthood they still prioritize protection, so self-control alone will not override automatic threat responses. Some networks share signals with memory centers, which means learned associations would sustain heightened feelings long after injury resolved. University imaging studies show overlap between threat response areas, emotion-processing hubs; those overlaps make cognitive effort less effective without targeted training. Shared expectations between partners often amplify response magnitude.
Use graded exposure sessions supervised by a clinician, paced activity plans with measurable goals, sleep optimization, brief cognitive reappraisal practice, partner education. Controlled trials at university centers reported median reductions of about 20–30% in self-reported distress when behavioral strategies were combined with skill training; another 15–25% improvement occurred after adding social support interventions. If you have research interest, review university protocols for cognitive approaches. Advocacy for workplace accommodations reduced symptom burden for many couples; structured communication helped partners know what support is needed.
A quick plan you can follow: assess baseline with simple daily log for at least 2 weeks, set one measurable goal per week, practice breathing 2x daily plus 3x during flare-ups, schedule one session with clinician within 4 weeks, ask for workplace advocacy when needs exceed routine capacity. For yourself, shed unhelpful expectations about willpower; accept that some urges will persist, use strategies to reduce reactivity so feelings become less overwhelming. Identify triggers, note what calms them, review logs weekly; always preserve rest periods, limit high-demand tasks to less than 50% of available energy early in recovery. A little clinical advocacy would yield a tremendous reduction in functional limitations for many, much faster than reliance on willpower alone. Those who track triggers know what increases distress much more clearly, which lets them choose tailored activities that release tension rather than increase threat response.


 Douleur et Votre Cerveau – Comprendre le Lien">
Douleur et Votre Cerveau – Comprendre le Lien">

 How to Build Daily Love in Your Marriage with Small Acts">
How to Build Daily Love in Your Marriage with Small Acts">
 5 Dating Advice Mistakes That Are Ruining Your Chances of Finding Love">
5 Dating Advice Mistakes That Are Ruining Your Chances of Finding Love">
 Am I Too Traumatized to Be in a Relationship? Signs & Recovery">
Am I Too Traumatized to Be in a Relationship? Signs & Recovery">
 How to Practice Emotional Intelligence in Relationships – 8 Practical Tips">
How to Practice Emotional Intelligence in Relationships – 8 Practical Tips">
 How Social Media Is Affecting Relationships — Impact & Tips">
How Social Media Is Affecting Relationships — Impact & Tips">
 4 Raisons Pour Lesquelles Vous Détestez et Êtes Jaloux des Autres — Causes et Comment Surmonter">
4 Raisons Pour Lesquelles Vous Détestez et Êtes Jaloux des Autres — Causes et Comment Surmonter">
 1500 Personnes Partagent des Conseils en Matière de Relations – Conseils Essentiels pour l’Amour">
1500 Personnes Partagent des Conseils en Matière de Relations – Conseils Essentiels pour l’Amour">
 Embrace the Mud – Guide ultime des courses dans la boue, du plaisir en plein air et du bien-être">
Embrace the Mud – Guide ultime des courses dans la boue, du plaisir en plein air et du bien-être">
 5 Proven Secrets to Make People Like You Fast | Social Skills">
5 Proven Secrets to Make People Like You Fast | Social Skills">
 15 signes que vous êtes intellectuellement compatibles avec votre partenaire">
15 signes que vous êtes intellectuellement compatibles avec votre partenaire">