Prioritize immediate safety: establish an exit plan, keep keys and phone in a consistent, accessible spot, share a code word with a trusted friend or neighbor, and contact authorities if any threat of physical harm appears. Carry a small emergency kit and store copies of identification and critical documents outside the shared residence so separation is possible at short notice.
Track incidents precisely: log date, time, triggers (for example, arguments after a partner has been drunk), specific words or actions, and visible injuries or property damage. In one case, steven discovered a pattern of escalation linked to late-night drinking; that record allowed legal advocates to treat events as repeated harm rather than isolated outbursts. Consistent logs help survivors qualify for protective orders and determine whether anger is actually controlled or symptomatic of deeper issues.
Communicate boundaries with measurable terms: state non-negotiables (no hitting, no threats, no property destruction) and specify consequences (temporary separation, calling a mediator, or filing reports). Avoid reflexive agreeing during escalation – agreeing to placate often reinforces the behavior and can result in more severe episodes later. Evaluate whether the partner’s outbursts reflect temperament, deep-seated trauma, or unrealistic expectations; categorize reactions as disproportionate, situational, or deliberately abusive to inform next steps.
Set concrete supports and options: use documented evidence for counselors and courts, schedule individual therapy for both parties if safe, and involve trained advocates before attempting joint sessions. If children are involved, create a custody and safety plan that prioritizes their ability to live in a stable environment. Expect measurable outcomes: enforced boundaries often reduce frequency of incidents, while repeated abuse typically requires legal separation to survive and rebuild well-being.
Recognize Patterns and Immediate Risks
Assess imminent danger: exit the area and call emergency services if hitting, beating, choking, or weapon use occurs.
Log repeated acts with dates and brief descriptions; catalog origin of each episode (stressors, substance use, past trauma) to map escalation frequency and triggers.
Monitor responses during conflict: taking feedback badly, sudden silence when conversation goes toward accountability, or loss of inhibitions under alcohol/drugs all raise immediate risk.
Note self-directed signals: they may blame themselves, display visible shame, or oscillate between blaming others and minimizing harm; that pattern affects capacity for genuine repair.
Decide specific thresholds for action: physical contact, property damage, threats, or stalking require separation and outside help; outside intervention is needed before patterns normalize.
Use social resources: inform trusted contacts, workplace security, or local services; articles and community listings provide concrete ways to prevent recurrence and document incidents for authorities.
Assess willingness to change: absence of sustained engagement in counseling, refusal to accept responsibility, or repeated denials reduce realistic hope for rapid change; everyone around should have a safety plan.
Compare contexts from different settings and view third-party reports; prior experience of betrayal or violence increases risk and makes protective measures justifiable rather than optional.
Preserve evidence: timestamp messages, save photos, obtain medical records, and avoid reactive blaming during incidents; keep records that show patterns and make vulnerable periods visible to professionals.
| サイン | Risk level | Immediate action |
| Physical contact or beating | 高い | Leave immediately; call police; seek medical care |
| Threats or stalking | 高い | Document, obtain protection order, alert workplace |
| Substance-fueled loss of inhibitions | Moderate–High | Limit contact during intoxication; set boundaries; involve support network |
| Repeated minimization or blaming | Moderate | Require professional assessment; decide on safety boundaries |
Track specific triggers: how to log incidents and spot repeat situations
Create an incident log template and record events immediately: date, exact time, location, trigger (words/actions), sequence of events, your immediate response, outcome, witnesses, and a severity score from 1 to 10. The template must include a short field for “what was said” and another for “how it felt” so entries capture both facts and internal reaction; if an entry doesnt capture something, add a follow-up note rather than deleting the original. Always timestamp entries and store copies in two places (encrypted cloud and a local export) to preserve evidence and preserve freedom of information.
Categorize each item with tags such as: financial, parenting, work-stress, alcohol, jealousy, past-trauma. Mark items that relate to marriage or wider family separately and flag anything that meets legal definitions of abuse (threats, physical harm, sexual coercion). Distinguish a verbal outburst from sustained controlling behavior: an outburst is short, sharp, often situational; control is repetitive, planned, and sets limits on choices. Note whether the incident was bringing up previous incidents or somewhere connected to past events – that perspective helps avoid discounting patterns as isolated.
Review the log at fixed intervals: run a weekly tally and a monthly frequency chart. Calculate: total incidents, incidents per trigger tag, average severity, and number of incidents that resulted in escalation (police, medical visit, threats). Establish thresholds that trigger action – for example, three recorded threats in 30 days, or any incident with physical harm, requires contacting resources and activating a safety plan. If patterns show rising severity or control, decide on next steps (legal advice, leaving, emergency shelter) rather than waiting until ready; planning increases options to survive and preserve children and self.
Use concrete formats: spreadsheet columns (date,time,location,trigger,preceding-event,body-language,verbatim-quote,severity,action-taken,witness,follow-up), or a simple app that exports CSV. Create a short coded phrase to share with trusted family so others listen and can intervene. Keep a list of local resources and hotlines inside the log file. Sample quick entry: “2025-09-12, 20:15, kitchen, money argument, said ‘you never’, felt trembling, severity 7, partner slammed door, left room, no police, told friend next day.” That example demonstrates how to capture facts, feelings, and immediate ways of staying safe rather than arguing or trying to change the other person on the spot.
Use the log to generate ideas for boundary work: note which interventions reduced escalation (pausing conversation, exiting room, calling a mediator) and which made things worse (matching tone, public confrontation, bringing up unrelated past incidents). Track whether attempts to set limits were respected or discounted and whether the pattern looks dysfunctional or deliberately harmful. If entries show almost constant attempts to control, or repeated threats to fight or to restrict freedom, escalate to professional support without delay.
Assess short-term safety: steps to take when a moment turns volatile
Immediately move to an exit-accessible place, lock the door, create distance, and call emergency services or a prearranged contact if danger escalates.
- Identify exits and safe rooms; keep phone, keys, and a small emergency bag accessible so a quick move is possible.
- If partner is drunk or impaired, treat risk as higher; remove children to a different room or to parents/adults not involved to minimize exposure.
- Set clear boundaries with short assertiveness phrases; limit talking to essential instructions and refrain from arguing or trading hurtful remarks that escalate interaction.
- Use a code word with a trusted friend or family member; send location via phone or computer only if doing so does not increase risk.
- Document the incident immediately after reaching safety: note times, dates, injuries, exact words used, and keep screenshots or recordings as evidence.
- Avoid rooms with potential weapons (kitchen, garage); step back if tension goes up, move to public or well-lit areas within the place if leaving is not yet possible.
- If children are present, prioritize their safety because exposure to abuse or aggressive behavior affects development and can mirror patterns raised in childhood or origin trauma.
- Plan short exits: identify where to live temporarily (parents, girlfriend, husband, shelter), pack ID and medications, and decide who will transport belongings so leaving later is faster and safer.
- After immediate safety is secured, contact local resources: hotlines, shelter networks, or legal advocates who can recommend protective orders and next steps; Virginia residents can access state-specific listings through local social services.
- Track behavior differences over time and collect part-by-part evidence that shows patterns rather than isolated claims; an advocate can help fully assemble documentation for police or court.
- Do not match insults or attempt to justify retaliation; restraint and de-escalation preserve safety and make later legal or support actions stronger and more credible.
- If feeling insecure about decisions, find a trusted advocate or counselor to discuss options; small practical steps (sleep, nutrition, stronger support contacts) help survive the short term and make longer-term plans for a happier, safer life.
Resource: National Domestic Violence Hotline – 24/7 support, shelter referrals, and local resources.
Identify escalation signs that mean you should pause the conversation
Pause the conversation immediately if raised volume, repeated blame, or physical aggression are seen; specific red flags include shouting that keeps escalating beyond two minutes, throwing objects, clenched fists, stepping physically toward another person, or smelling alcohol on breath.
Clear actions: step away 15–30 minutes, move children along to a safe room in the home, and state a short stop phrase such as “I stop now; we will talk later.” If husband or another family member appears intoxicated or becomes verbally abusive, prioritize safety and remove vulnerable people rather than trying to reason in the moment.
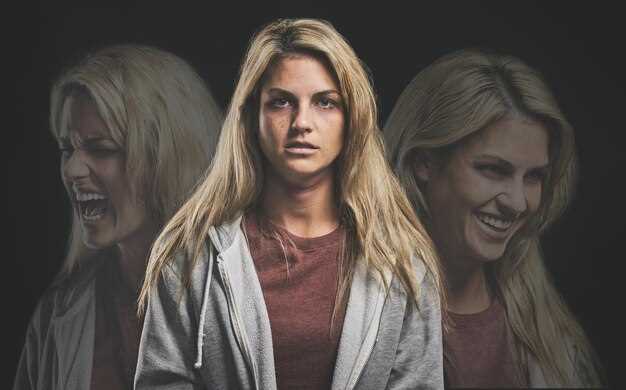
Watch emotional signals: sudden withdrawal, crying, explosive tears, or stubborn silence are emotionally charged cues that the conversation is no longer productive. Seeing past patterns–learned responses from childhood, expressed rage tied to old wounds, or long-standing frustration that keeps resurfacing–indicates a dysfunctional cycle rather than a solvable conflict in that moment.
Set concrete boundaries: only resume discussion once both parties are calm and cool for at least 20–60 minutes, not immediately after a flare-up. Recommend documenting what was said and seen, seek outside support when patterns are strong, and create a safety plan for home if threats or physical harm appear. Repeated escalation risks losing emotional stability, long-term health, and a constructive view of family life; treat any signs of physical aggression as an emergency.
Distinguish between repeated harmful behavior and isolated outbursts
Keep a dated incident log and collect corroborating evidence: record trigger, verbatim quotes, physical actions, witness names, photos and medical notes; classify a pattern if 3 or more harmful acts in six months or any physical assault.
Usually adults practicing systematic logging prevent disputes over facts and can present objective evidence rather than only impressions; keep copies off-site and timestamped so this record supports decisions with clear data.
Isolated outbursts are often loud and reactive, end quickly, and do not repeat the same harm; repeated harmful behavior goes beyond single episodes when the actor acts with higher frequency, cycles through aggression, or escalates into threats or vicious damage – telling patterns include similar triggers, identical language, or escalating reaction that sets an unsafe tone in interaction. However, severity and frequency should be measured quantitatively (incidents per month, injury score, witness corroboration) instead of relying on memory alone.
If a pattern is confirmed, enact safety steps: tell closest family members, befriend neutral supporters, move important documents somewhere secure, plan to live separately if threats persist, contact national hotlines or local authorities, and archive every threatening conversation as evidence; document everything related to incidents so records lead to clearer legal options. These steps protect loved family members and preserve choices for future stability, then seek clinical assessment and legal advice as needed.
This article supplies numeric thresholds, documentation templates and referral steps that set clear boundaries and reduce risk.
Create a short de-escalation script you can use in the moment

Lower voice, pause for three deep breaths, and use this exact three-line script to diffuse escalation immediately.
Line 1 – Name the behavior: “I hear the tone and the frustration; recent experiences suggest this outburst is tied to something bigger.”
Line 2 – Set a boundary and offer a minimal option: “I need a short pause. Choice: pause five minutes or continue now with calm rules.”
Line 3 – Invite origin and repair: “I want to know what led to this, because understanding the origin helps work on habitual patterns and safer expression later.”
Example: “hassan, I see the shame and tightness; sometimes that shame brings aggression. A five-minute break can diffuse the pressure and prevent a verbal beating.”
Tone affects responses; do not respond with passive silence, since passive moves often makes the other side stronger and fuels escalation. Repeating the same defensive fight pattern harms trust over a year of interactions. The role during de-escalation includes holding a fair boundary, using empathy to name feelings on each side, and avoiding anything that will play into aggression. Effective dealing requires clear limits, brief choices, and follow-up work.


 怒っている人を愛する時 – 対処戦略と人間関係のヒント">
怒っている人を愛する時 – 対処戦略と人間関係のヒント">

 結婚生活に日々の愛を育む小さな行い方">
結婚生活に日々の愛を育む小さな行い方">
 恋愛のチャンスを潰している5つのデートのアドバイスの間違い">
恋愛のチャンスを潰している5つのデートのアドバイスの間違い">
 トラウマを抱えすぎていると恋愛はできない?兆候と回復">
トラウマを抱えすぎていると恋愛はできない?兆候と回復">
 人間関係において感情的知性を実践する方法 – 8つの実用的なヒント">
人間関係において感情的知性を実践する方法 – 8つの実用的なヒント">
 ソーシャルメディアが人間関係に与える影響 — 影響とヒント">
ソーシャルメディアが人間関係に与える影響 — 影響とヒント">
 他者を憎み、嫉妬する4つの理由 — 原因と克服方法">
他者を憎み、嫉妬する4つの理由 — 原因と克服方法">
 1500 人が共有する恋愛アドバイス – 愛に役立つ重要なヒント">
1500 人が共有する恋愛アドバイス – 愛に役立つ重要なヒント">
 Embrace the Mud – Ultimate Guide to Mud Runs, Outdoor Fun & Wellness">
Embrace the Mud – Ultimate Guide to Mud Runs, Outdoor Fun & Wellness">
 5つの実証済みの秘訣で、人々がすぐにあなたを好きになる方法 | コミュニケーションスキル">
5つの実証済みの秘訣で、人々がすぐにあなたを好きになる方法 | コミュニケーションスキル">
 15 Signs You’re Intellectually Compatible With Your Partner">
15 Signs You’re Intellectually Compatible With Your Partner">