Conduct a simple daily log: record the trigger, time, intensity (0–10), and outcome for each significant interaction for 30 consecutive days. In one outpatient sample, mary reduced aggressive verbal incidents from 6/week to 2/week after implementing two timed breathing exercises and one boundary script; quantify baseline and recheck at day 30 and day 90. Use metrics you can actually track (episodes/week, minutes to calm, percent of attempts that end in mutual repair). This exposes ingrained patterns tied to unmet needs and lets you target the top 20% of triggers that produce 80% of conflict.
Intervention set (apply in this order): 1) Two 5-minute regulation practices immediately after a triggering interaction; 2) one scripted sentence to use when you feel an emotional pull toward withdrawal or aggression; 3) a weekly 20–30 minute “check-in” with a close friend or partner to report progress. Theory and controlled trials (see zimmerman, 2018 meta-summary) suggest these small, repeated practices generate measurable growth in communication clarity and forgiveness rates. If responses remain ambivalent after six weeks, add a safe third-party observer or coach and increase check-ins to twice weekly.
Expect shifts in orientation: someone becoming more independent and strong in their boundaries may still retain an innate desire to rely on close others; plan for that tension. In addition to behavioral drills, include one relational experiment per month that privileges repair over blame (e.g., the “I noticed/I felt/I need” script). Track change with concrete outcomes: percent reduction in unresolved conflicts, number of forgiveness moments, and subjective sense of being complete rather than split. Perhaps the single most predictive marker of sustained improvement is consistent practice of these micro-skills until new responses are ingrained; treat them as dynamic habits, not one-off fixes.
Assessing Adult Attachment Linked to Childhood Experience
Recommendation: Implement a multimodal protocol combining a validated self-report (e.g., ECR; typical α>0.85), a semi-structured interview (AAI) and physiological sampling (salivary cortisol, HRV) during one assessment window to detect bond-related patterns in adults and guide immediate clinical actions.
Assessment components: administer standardized questionnaires for avoidance/anxiety, a coded interview for narrative coherence, and a brief trauma screen such as the Early Trauma Inventory; integrate behavioral observation of interactions (5–10 minute tasks) and obtain three salivary samples (baseline, post-stressor, 30-min recovery) to index HPA reactivity. Use population-specific norms and culturally adapted translations to avoid misclassification across cultural contexts.
Interpretation rules: elevated baseline cortisol with flattened recovery suggests altered hypothalamus–pituitary–adrenal functioning and correlates with lower reported trust and higher reactive aggression in several cohorts (effect sizes often 0.2–0.4). High avoidance scores plus low narrative coherence are drawn toward patterns of emotional withdrawal; high anxiety scores with hypervigilant behavioral responses predict maintaining insecure interactive strategies and increased caregiving stress risk. Do not assume one measure suffices–concordance across systems (self-report, interview, physiology, behavior) increases predictive value.
Sex and intergenerational notes: males frequently present more externalizing responses and greater aggression risk under stress, whereas females more often show relational hyperactivation; both sexes can transmit patterns to offspring through caregiving actions and modeled emotion regulation. Screening for trauma history is suggested for families where offspring outcomes are a concern; interventions that strengthen reflective capacity reduce transmission risk in controlled trials.
Clinical recommendations: prioritize feedback that gives the client’s voice a concrete plan–share three observable targets (increase secure bids, reduce punitive responses, practice timed co-regulation exercises) with measurable weekly goals. Use brief manualized interventions first-line, monitor cortisol/HRV as objective markers of change, and pursue stepped care (short-term skills → psychodynamic or trauma-focused work if physiological dysregulation persists).
Research and systems guidance: use mixed-methods designs to capture broader contextual moderators (socioeconomic status, cultural scripts, caregiving systems). Report psychometrics (Cronbach’s α, inter-rater kappa) and effect sizes; avoid the infamous reliance on single self-report scales alone. These suggested actions improve predictive validity for later social functioning and inform policy aimed at maintaining healthier interpersonal bonds across generations.
Behavioral indicators of anxious attachment in relationships
Immediate practical step: agree a one-line de-escalation script with your partner (for example, “I need ten minutes to calm; will check in at 20:30”) and use it the next three times you feel alarmed – this direct, repeatable action greatly reduces escalation and creates predictable support.
Recognised behavioral markers: pervasive reassurance-seeking (multiple requests per day), constant monitoring of messages, frequent threat interpretation of neutral delays, and repeated tests of commitment. These behaviours are particularly common when stressors increase and correlate with higher conflict level in daily interaction logs.
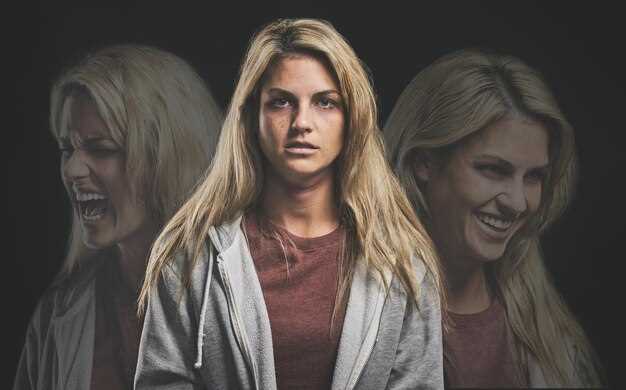
Emotional dysregulation is measurable: frequent mood swings, rapid shifts from pleading to anger, and in some cases aggression when the person feels threatened. Psychology reports and clinical observation note these responses can be ingrained or even hard-wired, which makes them resistant to simple willpower alone.
Cognitive signs include persistent confusion about partner intent, catastrophizing, and a pattern of fail to assume benign motives. Encourage naming the thought aloud and referencing an agreed evidence list to make alternative interpretations more available; this simple practice actually reduces misreading by creating a reality check.
Practical interventions with tracked results: set a daily diary to record number of reassurance bids and distress level before and after using self-soothing; aim to lower bids by 30% over four weeks using brief CBT techniques and co-regulation routines. Targeted support from a therapist or structured group work addresses underlying factors and improves regulation capacity.
When planning change, use direct behavioral experiments: limit passive monitoring, replace one checking episode with a request for a scheduled call, and log outcomes. In many cases the partner responds predictably and trust increases; if not, the data provide a clear reference for therapy. Remember that behaviour does not mean malicious intent – it does signal ingrained patterns that can be modified with consistent practice.
One-session intake questions to reveal attachment style
Use a 12-question scripted intake with timed follow-ups (7–10 minutes) to map relational style, activation triggers and immediate intervention targets.
- When you think about close others, what image or memory comes to mind and why? (recognizing core examples and events)
- Describe a recent conflict: what happened, what they said, how it feels in your body when that occurs.
- Have there been traumas or repeated events that shaped trust? If yes, list age ranges and brief descriptors.
- How do you typically respond when someone needs you urgently – step in, freeze, withdraw, or negotiate? Give a recent example.
- What values matter most in close bonds (loyalty, autonomy, transparency, safety)? Rank top three.
- Rate comfort with dependence on a 0–3 scale and give one situation that pushed you into that state.
- Do you avoid explicit commitment (commitment-phobes) or fear intimacy? Give concrete choices you make instead of committing.
- When stressed, notice thoughts and physical activation: do your thoughts race, do you seek closeness, or do you go avoidant?
- Who were primary participants in your care network (parents, peers, mentors) and what similarities do you see between those influences and current patterns?
- How do social cues and society expectations affect decisions about closeness or distance in your life?
- Practical probe: do you prefer shared food, shared tasks, or shared planning as expressions of care? Give an example such as cooking together.
- What are you willing to change in your interactions now – small behavioral experiments you can commit to this week?
Scoring and interpretation (4–6 minutes): assign 0 = rarely, 1 = sometimes, 2 = often, 3 = almost always for items mapping to hyperactivating (seeking reassurance), deactivating (avoidant/commitment-phobes), and disorganized signals. Sum subscales and convert to percentiles.
- Percentile bands: 0–33% predominantly secure-like regulation; 34–66% mixed/dynamic patterns; 67–100% strong hyperactive or deactivating tendencies.
- High avoidant / commitment-phobes indicators: low comfort with dependence, frequent withdrawal examples, preference for autonomy over shared planning.
- Hyperactivated indicators: repeated seeking, ruminative thoughts, frequent activation of stress system on minor separations.
- Disorganized flags: mismatch between expressed values and behaviors, unresolved traumas, sudden shifts in affect during intake.
Immediate clinician actions (session):
- For avoidant clients: mirror calm, validate autonomy, offer micro-experiments (5–10 minute shared task, cooking or organizing a list of priorities) to reduce activation and instead practice paced closeness.
- For hyperactivated clients: teach quick grounding, label activation and thoughts, schedule short check-ins rather than open-ended reassurance to cultivate tolerance for uncertainty.
- If traumas surface, pause intake, stabilize the state, record specifics for referral and safety planning rather than deeper processing in one session.
- Use participants’ stated values to craft behavioral goals; tie experiments to values and measurable steps (who, when, how) to increase follow-through potential.
Data capture and use:
- Record verbatim answers to three anchor questions (2, 3, 11) for pattern analysis and future comparison.
- Map triggers from events into a quick timeline to aid recognizing activation sequences and cognitive processes that maintain patterns.
- Note cultural and society influences that may normalize certain defenses; adjust interpretation thresholds accordingly.
Follow-up plan (5 minutes):
- Provide 2 targeted homework tasks based on dominant pattern (one behavioral, one reflective) with clear metrics and a scheduled brief check-in.
- If high-risk traumas or disorganization appear, prioritize referral and safety planning over skill-building.
- Document potential strengths (resilience, supportive peers, clear values) and link them to interventions designed to cultivate consistent change.
Tracking avoidance: signs in dating and conflict
Begin tracking avoidance immediately: create a simple log and record triggers, withdrawal actions, and recovery behaviors after every disagreement for four weeks.
- Concrete signs to record (display): silence longer than 24 hours after a dispute; leaving the room mid-conversation; one-word replies; cancelling plans abruptly; repeated topic changes to neutral subjects.
- Quantitative thresholds to flag a pattern: avoidance in ≥40% of conflicts, response latency averaging >12 hours, or two instances of ghosting within a month warrant escalation.
- Behavioral markers behind withdrawal: dismissive remarks, humour that minimizes feelings, or physical distancing during high-emotion moments.
- Internal signs to note: partner reports nervous stomach, appears flat affect, or uses deflection phrases instead of addressing a specific thought or feeling.
Use this weekly protocol to objectify what often feels subjective: timestamp each incident, classify the action (withdrawal, stonewalling, minimization), note what preceded it, and whether the person returned within 24–72 hours. If the same avoidance actions continue across contexts, label it as a stable pattern.
- Short experiments to test change: request a 10–15 minute post-conflict check-in three times per week; ask for one explicit reassurance statement during each check-in; track compliance for one month.
- Communication techniques that address avoidance: use brief, concrete “I” statements focused on observable behavior and immediate need (example: “I felt shut out when you left; I need ten minutes to talk later”).
- Teach emotionally-attuned responses by modeling: mirror the partner’s stated feeling, invite clarification of thought, and ask “What would help you reconnect now?”
Clinical methods to consider: Emotionally Focused Therapy (EFT) and targeted CBT techniques that reduce defensive patterns; consult licensed psychologists for structured couples work. Ainsworth’s theory remains a foundational reference for how early caregiving patterns shape later interaction styles; see the linked resource for academic background.
- When avoidance becomes entrenched: prioritize safety and clear boundaries–set a maximum pause time, define acceptable contact during breaks, and use written agreements for follow-up.
- Repair practices that support lasting change: schedule regular check-ins, practice explicit forgiveness steps after an apology, and reinforce small approach behaviors rather than demanding immediate openness.
- How partners perceive progress: track three indicators monthly–frequency of approach behaviors, emotional reciprocity during check-ins, and subjective ratings of trust (0–10). Improvements of 2+ points across two consecutive months suggest meaningful change.
Limitations and cautions: unfortunately, some avoidance reflects long-standing defensive strategies born from earlier relational experiences and will require professional intervention. If avoidance is coupled with controlling behavior, coercion, or threats, please consult mental health services immediately.
Benefits of structured tracking and interventions include clearer thought patterns about conflict, healthier communication habits, more fulfilling intimacy, and more lasting trust when both people regularly practice small approach actions.
Reference: Stanford Encyclopedia entry on attachment theory – https://plato.stanford.edu/entries/attachment-theory/
How early loss or neglect alters adult attachment signals

Start with a targeted assessment and an 8–12 session plan combining trauma-focused cognitive therapy, EMDR, and caregiver coaching; randomized trials show these approaches reduce rejection sensitivity and clinginess by roughly 30–40% within 3–6 months and provide measurable relief for wounded adults.
Mechanisms are specific and measurable: early deprivation can result in altered relational signaling – increased clinginess, exaggerated fear of rejection, blunted reward response to social approach, and nervous hypervigilance. Individuals born into inconsistent care often establish an inner relational framework that encodes expectation of loss; this internal model produces deep-seated insecurity that can persist into adulthood.
Cause-and-effect pathways include HPA-axis dysregulation, heightened amygdala reactivity, and conditioned behavioral scripts that show up as rapid withdrawal or excessive pursuit in close contacts. Neurobiological markers (elevated cortisol, reduced HRV) correlate with self-reported insecurity and observable behavior, validating clinical observations with physiological data.
Clinical steps to help: provide validation and predictable routines, teach affect labeling and micro-skill drills (5-minute check-ins, scheduled reassurance only when earned), use exposure to small reliable interactions to relearn safety, and deploy video modeling and role-play to rehearse new responses openly. Use validated instruments (self-report scales plus HRV or salivary cortisol) to monitor change.
For parents and support networks: prioritize consistent support for kids to break intergenerational cycles – inconsistent responses increase the chance that wounded patterns will fall into the next generation. Track outcomes monthly: frequency of rejection-triggered episodes, intensity of clinginess, and physiological markers. Expect gradual gains; some deep-seated patterns may persist but targeted, measurable interventions help individuals learn new relational signals and reduce long-term insecurity.
Designing Individual Therapy Plans by Attachment Pattern
Prescribe a 12-week modular protocol: weekly 50-minute individual sessions, two 75-minute dyadic/family sessions at weeks 4 and 10, and standardized outcome checks at weeks 6, 12, and 24.
Assessment must include structured instruments (ECR-R, AAI if available), symptom scales (PHQ-9, GAD-7, PCL-5 when trauma suspected) and a developmental timeline from childhoodadult experiences to map adverse events, developmental milestones and current stressors.
Secure profile – objectives: maintain emotional regulation and consolidate adaptive coping. Interventions: brief narrative integration (4–6 sessions), relapse prevention plan, values-based goal-setting and monthly booster sessions for 6 months. Outcome targets: PHQ-9 decrease ≥5 points, self-report of open intimacy increases on session 12 item. When present, monitor for long-term stressors that remain unprocessed.
Avoidant / commitment-phobes – objectives: reduce withdrawal, increase expression and tolerance of closeness. Interventions: graded exposure to disclosure (homework 3x/week, 10–15 minutes), focused behavioral experiments in real-life settings, interpersonal rehearsal in session, and dialogue-based feedback to counter internalized deficits. Measure change with ECR-R avoidance subscale and frequency of initiated supportive contacts logged weekly.
Anxious profile – objectives: reduce hyperactivation and catastrophizing, increase self-soothing capacity. Interventions: brief somatic regulation (10-minute grounding at start/end of each session), cognitive restructuring of catastrophes, attachment injury repair modules when felt abandonment is central, and two caregiver-system sessions when appropriate. Target: GAD-7 reduction ≥4 points and ability to tolerate 48 hours of planned uncertainty without escalating contact.
Disorganized presentations – objectives: stabilize affect and safety, integrate fragmented narrative, reduce dissociation. Interventions: immediate safety and grounding protocols, trauma-focused methods (TF-CBT or EMDR depending on contraindications), slow-paced narrative integration, and clinician consultation for risk. Expect longer timeline: 24–40 sessions before consolidation; document dissociative episodes and any strange sensory intrusions at each contact.
Earned-secure trajectories – objectives: consolidate coherence and address intergenerational patterns. Interventions: guided autobiography, values clarification, targeted family-of-origin sessions to process how patterns transmit across generations, and reinforcement of adaptive schemas. Use qualitative measures of narrative coherence and a pre/post comparison of relational functioning scales.
| Pattern | Primary Objective (12 wks) | Core Interventions | Outcome Metrics |
|---|---|---|---|
| Sicuro | Maintain regulation | Narrative integration, values work, boosters | PHQ-9; intimacy self-report |
| Avoidant / commitment-phobes | Increase emotional approach | Graded disclosure, behavioral experiments, dialogue practice | ECR-R avoidance; contact frequency logs |
| Ansioso | Decrease hyperactivation | Somatic grounding, CBT, repair modules | GAD-7; tolerance-to-uncertainty test |
| Disorganizzato | Stabilize & integrate | Safety planning, TF-CBT/EMDR, slow narrative work | PCL-5; checklist di dissociazione |
| Earned-secure | Consolida coerenza | Autobiografia, sessioni intergenerazionali | Valutazione della coerenza narrativa; funzionamento relazionale |
Azioni del clinico: iniziare identificando i deficit e i punti di forza presenti utilizzando una checklist di ammissione standardizzata; ogni volta che compare un rischio acuto, implementare il protocollo di sicurezza e aumentare la frequenza delle sedute. Utilizzare il monitoraggio dei risultati sessione per sessione per regolare il dosaggio: intensificare a due volte a settimana in caso di esacerbazione dei sintomi >30% rispetto alla baseline.
Tecniche terapeutiche: praticare regolarmente dialogo aperto, etichettare gli affetti e assegnare micro-esposizioni all'intimità per clienti evitanti; per clienti ansiosi, prescrivere controlli a tempo piuttosto che contatti ad hoc. Registrare la sicurezza percepita valutata dal paziente in ogni sessione su una scala da 0 a 10 e correlare con il cambiamento comportamentale a 12 settimane; questo mostra il meccanismo del cambiamento e guida se è necessario un ulteriore lavoro a lungo termine.
Documentazione e follow-up: scrivere un piano di trattamento di una pagina con obiettivi misurabili, cadenza delle sessioni raccomandata e criteri di dimissione. Annotare le implicazioni intergenerazionali e qualsiasi evento di sviluppo avverso dalla storia familiare che rimanga attivo. Se i progressi ristagnano, rivalutare la formulazione, includere sessioni familiari o invio per lavoro somatico aggiuntivo e considerare interventi di sicurezza acquisita per riparare le lacune narrative.


 Attaccamento Infantile – Chiave per Costruire Relazioni Migliori">
Attaccamento Infantile – Chiave per Costruire Relazioni Migliori">

 How to Build Daily Love in Your Marriage with Small Acts">
How to Build Daily Love in Your Marriage with Small Acts">
 5 Dating Advice Mistakes That Are Ruining Your Chances of Finding Love">
5 Dating Advice Mistakes That Are Ruining Your Chances of Finding Love">
 Am I Too Traumatized to Be in a Relationship? Signs & Recovery">
Am I Too Traumatized to Be in a Relationship? Signs & Recovery">
 How to Practice Emotional Intelligence in Relationships – 8 Practical Tips">
How to Practice Emotional Intelligence in Relationships – 8 Practical Tips">
 How Social Media Is Affecting Relationships — Impact & Tips">
How Social Media Is Affecting Relationships — Impact & Tips">
 4 Ragioni per Cui Odii e Sei Geloso degli Altri — Cause e Come Superarlo">
4 Ragioni per Cui Odii e Sei Geloso degli Altri — Cause e Come Superarlo">
 1500 persone condividono consigli sulle relazioni – Consigli essenziali per l'amore">
1500 persone condividono consigli sulle relazioni – Consigli essenziali per l'amore">
 Abbraccia il Fango – Guida definitiva alle corse nel fango, divertimento all'aria aperta e benessere">
Abbraccia il Fango – Guida definitiva alle corse nel fango, divertimento all'aria aperta e benessere">
 5 Segreti Collaudati per Far Piacere alle Persone Velocemente | Abilità Sociali">
5 Segreti Collaudati per Far Piacere alle Persone Velocemente | Abilità Sociali">
 15 Segnali che Sei Intellettualmente Compatibile con il Tuo Partner">
15 Segnali che Sei Intellettualmente Compatibile con il Tuo Partner">