Practical prescription: sit at a quiet center in your home, set a timer for 5 minutes, inhale for four seconds, exhale for six seconds, note sensations without judgment; repeat once more later in the day. This simple routine, when taken consistently for 6–8 weeks, creates a habit that yields measurable benefits for stress reduction.
Evidence summary from selected meta-analyses and randomized trials reviewed in clinical journals shows small-to-moderate effect sizes (Cohen’s d ≈0.3–0.6) for perceived stress reduction, with clinically relevant alleviating effects on anxiety scores. Studies that meet higher quality criteria report faster response in psychological symptoms, reduced rumination, improved attention metrics; physiology-level changes include shifts in autonomic balance, decreased inflammatory signals in several reports. Use these numbers as an accurate baseline for expected change over time.
Mechanisms documented with functional imaging reveal increased prefrontal regulation, reduced amygdala reactivity, altered connectivity in default mode networks; the difference in neural activation maps corresponds to improved emotional regulation, better task-focused performance. Clinically reviewed protocols that emphasize brief daily practice produce larger functional gains than sporadic, longer sessions taken infrequently, suggesting that time, not session length alone, determines cumulative benefit.
Selected, actionable techniques: 1) breath-centered noting – count inhales to five, reset when distraction occurs; 2) short physical-scan while seated – sweep attention across posture, shoulders, jaw, breath; 3) single-point attention during routine tasks – take three measured breaths before starting. Track session time, record comfort level, adjust posture to stay comfortable, review progress every two weeks to maintain habit-making momentum and to quantify overall change in your stress, sleep, focus.
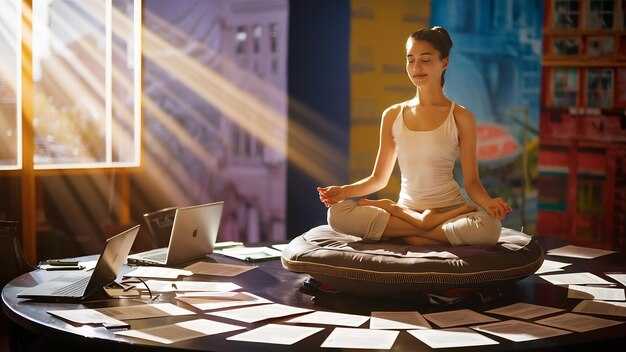
Practical Foundations: Getting Started with Meditation
Commit to 10–20 minutes of seated focused-breathing every morning for 30 consecutive days. Take three deep diaphragmatic breaths to settle; turn attention to the exhale with a light, steady focus, then settle here. Gently note when thoughts arise; label them briefly (“planning”, “worry”, “task”) then return to the breath. This protocol is easy to sustain for most beginners; after two weeks many report lower perceived stress.
Make an intentional choice of anchor; commit to that anchor for at least two weeks. The session involves clear parts: brief warm-up, anchor practice, short closing. Use a 4:6 inhale:exhale count for focused-breathing or a 10-minute body-scan split into 2–3 focused intervals. Small randomized trials with follow-up at 8 weeks reported increased telomerase-related markers in samples of 20–100 participants; immune markers in those studies were sometimes affected with reduced inflammatory signals.
Measure outcomes to track efficacy: use a sleep diary or wearable to log sleep duration, latency, awakenings; complete a validated stress questionnaire at baseline, after 4 weeks, follow-up at 8 weeks. Expect very modest effect sizes early; further improvements commonly appear after 8–12 weeks. For long-term disease risk the impact is multi-factorial; combine this practice with regular physical activity, improved nutrition, stable sleep hygiene to influence cardiometabolic health.
Support adherence through simple behav design: pair practice with an existing routine (tooth brushing, morning coffee), use cue-routine-reward loops, document streaks for reinforcement. Group sessions or short peer meetups increase retention in multiple trials. Build self-belief by recording measurable milestones: one-week blocks, three consecutive 10-minute days, then celebrate each block to strengthen reinforcement across different culture settings.
If drowsiness occurs, turn practice to a standing posture or use a 3-minute walking variant; if intrusive thoughts intensify, close eyes briefly then re-establish a light focus on breath. Settle here for the closing phase with five slow exhales as a warm-down. People with major psychiatric conditions may be affected differently; consult a clinician before beginning. Expect varied efficacy across individuals; benefits involve several parts of regulation: attention training, stress-reactivity shift, habit formation. After regular practice many report increased sleep quality, lower perceived stress, improved immune markers; long-term meditators in cohort samples often show associations with lower disease incidence though causality remains under study.
5-Minute Starter Routine for Busy Mornings or Evenings
Set a 5-minute timer, follow this exact sequence to stabilize mood, lower physiological arousal, sharpen attention.
| Time | Action | Purpose |
|---|---|---|
| 0:00–0:30 | Grounding breath: inhale 4, hold 2, exhale 6 | Vagal stimulation, immediate mood regulation |
| 0:30–1:30 | Brief body scan: note tension, release two areas | Lower muscle tension, increase interoceptive accuracy |
| 1:30–3:00 | Focused awareness on a neutral image or sensation, return when distracted | Attention training, reduce rumination |
| 3:00–4:00 | Label feeling with one word, rate intensity 0–10 | Emotion regulation via cognitive labeling |
| 4:00–5:00 | Set one intention for next time block, breathe three slow cycles | Goal priming, functional activation |
Perform seated, feet flat, spine neutral, shoulders soft; eyes open or closed, whichever keeps you safe while working.
Scholar-reviewed trials in small groups, including individuals with generalized anxiety disorder, report acute mood shifts, modest improvements over repeated sessions; reported efficacy ranges Cohen’s d 0.2–0.6 for self-report mood measures, larger effects for attention tasks, smaller effects for peripheral biomarkers.
Mechanisms from physiological mediators include increased vagal tone, lower cortisol, reduced inflammatory markers; these influence functional brain networks, shifting being from reactive toward regulated states, even reducing pathways that contribute to tissue damage such as necrosis in extreme cases.
Use meditative mindfulness techniques: anchor attention to breath or a neutral image, label feeling aloud or silently, return attention when thoughts drift; a small magnetic object used as tactile anchor can increase focus for some individuals.
Measure effect: record your feeling before session, after session, calculate change across an interval of seven days to assess efficacy; they who track small samples detect functional shifts faster, those who skip logs cannot judge progress.
If severe symptoms meet clinical thresholds, seek assessment, consult a clinician; short sessions remain a practical, low-time intervention useful for working schedules, whatever type or types fit their routine.
Guided vs. Unguided: Selecting the Right Format for You
Beginners should use guided audio in instructor-led sessions for 6–8 weeks; move to unguided only after sustaining 10–20 minute sessions without prompts.
Multiple randomized trials studied 8-week programs with daily practice; results shown include statistically significant reductions in perceived stress, effect sizes typically 0.4–0.8.
For chronic pain such as arthritis, group programs shown to reduce pain scores by roughly 10–30% across studies.
A practical schedule: every morning within 30 minutes of waking do a single 10–20 minute session; add short 3–5 minute intervals before public speaking or difficult contact.
Studies suggest shorter micro-sessions increase adherence when making a habit.
Allow a 30–60 minute interval after guided longer sessions to avoid fatigue.
Different type options include loving-kindness, breath-focused, body-scan; choose one which matches goals.
Combinations of guided plus unguided practice are often best; alternate guided sessions twice weekly with self-led practice three times weekly.
If you notice calmer baseline mood but drift in adherence, reduce duration to 5 minutes several times per day; this approach shown to raise long-term consistency.
To test formats for yourself, run 2-week blocks keeping total time identical; track mood, sleep, pain scores pre/post sessions.
Occasional group practice helps remind ourselves of realistic expectations.
For public groups pick instructors trained in trauma-sensitive cues; for those seeking immune support some programs studied reported increases in antiviral antibody response to vaccines.
For beginners with arthritis choose programs that include gentle movement; contact instructors about modifications.
Have an instructor lead early sessions until you can lead yourself.
Compare guided sessions to other formats before committing long term.
After going unguided for a month, record perceived changes; different individuals respond differently.
If undecided, probably begin guided; after 8–12 weeks reassess which format yields most benefits.
For functional integration into daily life use alarms, walking routes, habit stacking; make cues functional for you.
Breathwork for Quick Calm: Box Breathing, Equal Breathing, and 4-7-8
Use Box Breathing for immediate calm: inhale 4s, hold 4s, exhale 4s, hold 4s; perform 6–10 cycles while seated, breathe through the nose, monitor your heart rate for stabilization.
-
Box Breathing
- Protocol: 4-4-4-4 seconds; beginners may start with 3-3-3-3, progress by 1s every 3 sessions.
- Session dose: 2–5 minutes for acute stress; 10–20 minutes once daily to improve baseline reactivity.
- Physiology: works via vagal activation, slowing respiratory rate which reduces sympathetic tone; immediate HR variability gains often measurable within minutes.
- Practice tips: sit upright, soft gaze, use a timer; if lightheaded, reduce counts by 1s or pause after practice.
-
Equal Breathing (Sama Vritti)
- Protocol: inhale N seconds, exhale N seconds; common N values: 4, 5, 6; first choose what feels slow yet comfortable.
- Session dose: 5–15 minutes twice daily to improve sleep latency, daytime focus; slow progression minimizes dizziness.
- Mechanism notes: slow, even breathing alters CO2 levels progressively, affecting chemoreceptor feedback that modulates autonomic function; effects are multi-factorial, involving respiratory mechanics, cortical regulation, peripheral feedback.
- Who benefits: people with racing thoughts, insomnia; others who prefer continuous rhythm over holds.
-
4-7-8 (Relaxing Breath)
- Protocol: inhale 4s through nose, hold 7s, exhale 8s through mouth; repeat 4 cycles for immediate effect; extend to 8 cycles for deeper transition.
- Session dose: use as a rapid de-escalation tool before public speaking, stressful calls, sleep onset; avoid long holds if respiratory conditions exist.
- Practical caution: holds increase intrathoracic pressure; if chest discomfort occurs, shorten hold by 2s.
Evidence summary: several high-quality studies within structured programs such as mbsr report statistically significant reductions in perceived stress; some research notes potential methylation changes after sustained training, suggesting underlying epigenetic modulation rather than a single causal pathway. Neuroimaging work compares pre-post scans showing altered connectivity in regions tied to emotion regulation; while effect sizes vary, the literature suggests that benefits arise from combinations of breathing, attention training, slow physiological entrainment.
- How to choose a type: first evaluate tolerance for breath holds; if holds provoke anxiety, pick Equal Breathing; if rapid calming is needed, select Box Breathing; if sleep initiation is goal, try 4-7-8 after lights out.
- Progression plan: week 1 use 2–5 minute sessions twice daily; week 2 increase to 10 minutes once daily; after four weeks reassess symptoms, HR variability, sleep quality.
- Measurement suggestions: track resting pulse, subjective stress score, sleep latency; use simple logs every session for 30 days to detect statistically meaningful trends.
Contraindications: recent cardiac events, uncontrolled hypertension, severe pulmonary disease require clinician input; if dizziness occurs, stop, breathe normally, resume with shorter counts. For children, reduce counts by half.
- Tips for consistency: pair sessions with a fixed cue (waking, pre-sleep, coffee break); keep sessions short initially to increase adherence.
- Further combinations: combine Equal Breathing with brief progressive muscle release; alternate Box Breathing with paced walking for skill transfer to ambulatory stressors.
- What to expect after 2–8 weeks: many report improved sleep, reduced reactivity, clearer thinking; brains show slow shifts in functional connectivity; changes in stress biomarkers are usually gradual, reflecting multi-factorial adaptation rather than instant rewiring.
Final note: everyone can try these protocols; choose the best fit for current physiological state, progress slowly, consult a clinician for pre-existing medical issues, discuss further adjustments based on personal response.
Simple Metrics to Track Mood, Sleep, and Clarity
Record three numeric scores every day: mood 0–10, sleep quality 0–100, clarity 0–10; log only before bed, upon waking.
Mood: use a single-item mood score plus a short positive/negative affect checklist (3 positives, 3 negatives). A change ≥1 point on the 0–10 scale is clinically meaningful. Calculate a positive/negative ratio; a ratio <1 indicates negative bias. Add a single-item self-belief score 0–10 to track confidence shifts; decreases of ≥2 points warrant review. Aim for steadier, calmer baseline over two weeks.
Sleep: track Total Sleep Time (TST), Sleep Efficiency (SE), Sleep Latency (SL), Wake After Sleep Onset (WASO). Targets: TST 7–9 h, SE ≥85%, SL <20 min, WASO <30 min. Use actigraphy or validated sleep trackers nightly; combine with a short sleep diary entry before bed describing caffeine use, light exposure, pre-sleep routine. Dont average across heterogeneous nights without checking weekday/weekend states separately.
Clarity: use a 3–5 minute psychomotor vigilance test (PVT) weekly; median reaction time <250 ms indicates good vigilance for most adults. Add a brief Stroop-like accuracy test (30 trials) to detect cognitive control shifts. Track simple work-product markers such as typing speed or error rate for tasks relevant to your role; greater than 20% intra-week variability suggests impaired clarity.
Physiology & biomarkers: nightly resting HRV (RMSSD) and morning resting heart rate provide continuous objective markers. For research or clinical settings, measure telomerase activity and inflammatory cytokines including factor-α at baseline then every 3 months; reductions in factor-α often correlate with improved subjective scores (источник: scholar review). Telomerase increases have been reported in trials that reduce chronic stress; testing costs and lab access needs consideration.
Analysis rules: compute 7-day moving averages, weekly slopes, z-scores relative to a 30-day baseline. Look for consistent trends rather than single-day swings; a weekly slope improvement >0.1 z is fruitful. Pair subjective scores with at least one objective marker each week; this combination helps distinguish reporting bias from true physiological change.
Actionable plan: morning log for mood, nightly log for sleep, one short clarity test per week, continuous HRV nightly, biomarker panel every 3 months if available. Use these data to suggest targeted adjustments or therapies when trends show deterioration. Gently modify routines based on which marker shifts first; involve a clinician when biomarkers or clinical symptoms worsen. Here are thresholds to support decisions: mood drop ≥2 points over 7 days, SE <80% for two weeks, HRV decline >15% sustained; any of these does justify clinician contact.
Notes: combine subjective reports with objective markers to reduce bias, review their correlations monthly, dont ignore small consistent trends. This protocol supports mind-body work, helps prioritize interventions, helps build self-belief via measurable progress, supports various clinical therapies, supports greater resilience even when acute stressors are involved.
Integrating Meditation into Daily Life: Walking, Eating, and Transitions
Begin with 2–5 minutes of meditated walking: maintain 60–80 steps per minute, sync inhale for two steps then exhale for two steps; focus on footfall signals, torso resonance with breath. Duration guidance – minimal session 2 minutes, target 10 minutes twice daily; if attention drifts, note the thought then return to breath; dont force pace, keep gait healthy for joints; very short sessions still increase interoceptive awareness, producing a heightened sense of being.
For eating practice: before first bite pause 3–5 seconds, focus on breath then exhale fully; chew 20–30 times per mouthful, count bites to slow intake. Randomized trials report lower cytokine markers, modest reductions in ALT transaminase, improved immunity profiles with reduced inflammatory cells; moreover trials included functional imaging of brains, including increased connectivity in attention networks. These effects correlate with better glycemic control, healthier food choices, enhanced sense of well-being about hunger cues.
During transitions between tasks take three slow breaths: inhale 4 seconds then exhale 6 seconds; this 20–40 second resonance buffer shifts autonomic signals, improves heart rate variability, yields heightened attention when returning to work. Use phone reminders for minimal interruptions, dont multitask immediately after a meeting; figuring out timing reduces carryover stress, helps manage cortisol spikes further, produces better recovery for cognitive function, supports sustained being present throughout the day.