Reduce reactive outbursts now: pause for a 60-second paced-breathing reset, label the feeling aloud and state a simple behavioral aim (for example, “I feel angry; I will step back for two minutes”). This routine lowers sympathetic arousal, recruits frontal control and often prevents escalation.
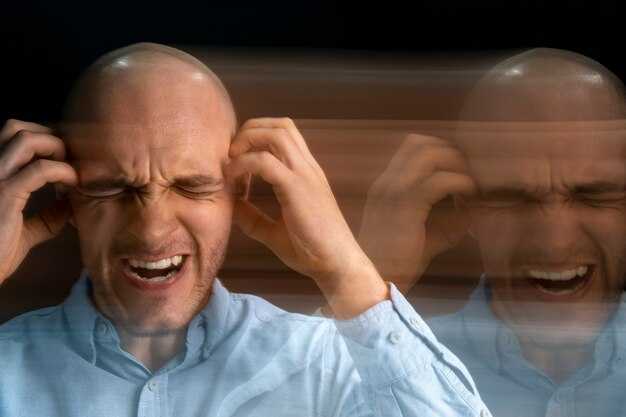
There are well-characterized neural systems that generate and regulate anger. Fast, evoked activity in the amygdala triggers the autonomic and endocrine cascade that can induce sweating, rapid heartbeat and a surge of adrenaline and cortisol. The principal mechanism for control sits in ventromedial and dorsolateral prefrontal cortex; when those regions underperform, reactive drives win. One calvo finding links heightened amygdala reactivity with weaker prefrontal recruitment in chronically irritable people, and imaging work shows covert aggression engages subcortical hubs even without visible behavior.
Different types of anger map to different patterns in brains and bodies and point to actionable steps to treat and improve outcomes. Acute threat responses respond to paced breathing and brief behavioral pauses; learned, provoked anger shifts with cognitive reappraisal and behavioural experiments; anger rooted in past trauma–common in people who were abused–requires trauma-focused approaches plus skills training to address underlying drivers. Drugs that boost serotonin reduce impulsive aggression, and combined therapy plus medication often produces larger gains. Track physiology (heart-rate monitors, short mood logs) to verify change, and use micro-practices of 30–90 seconds repeatedly: surprisingly small interventions produce measurable drops in self-reported anger within weeks.
Neural and bodily processes that produce an anger episode

When you feel anger rising, take six slow breaths per minute (5s inhale, 5s exhale) for two minutes: this immediate measure lowers heart rate variability (HRV) decline, reduces sympathetic drive and blunts amygdala reactivity enough to change behaviour in tens of seconds.
The sequence begins with rapid threat detection: sensory cortex and a subcortical route activate the amygdala, which sits at the centre of threat signalling and tags stimuli with 担心 or anger salience. Amygdala output triggers the hypothalamus and brainstem nuclei, engaging the sympathetic-adrenal-medullary (SAM) axis and releasing catecholamines within seconds; the hypothalamic–pituitary–adrenal (HPA) axis then raises cortisol, peaking roughly 20–30 minutes after onset. Prefrontal regions (ventromedial and dorsolateral PFC) exert top-down inhibition that modulates amygdala firing; reduced PFC recruitment correlates with loss of control and more severe outbursts.
Inside the body, these neural events produce measurable changes: heart rate often increases by 10–30 beats per minute, blood pressure rises, skin conductance increases, pupils dilate and skeletal muscle tone increases–EMG shows rapid activation in facial and arm muscles, which explains why people become ready for hitting or fleeing. Interoceptive signals coded by the insula amplify subjective anger and drive emotional behaviour. These peripheral measures are useful markers in experiments and clinical monitoring.
Laboratory tasks that provoke anger use provocation or lexical interference (for example, insult-laden lexical Stroop tasks) to compare neural responses; fMRI shows amygdala and anterior cingulate cortex activation within tens to hundreds of milliseconds, while PFC modulation appears subsequently. Studies done with physiological recordings report decreased HRV and increased skin conductance frequently during episodes; these measures correlate with self-reported intensity and behavioural aggression.
Individual differences matter: sensitivity to threat, past trauma and ptsd produce higher baseline amygdala reactivity and lower PFC control, explaining why some individuals escalate faster and experience more severe, prolonged episodes. Differences between PTSD and control groups appear in both neural activation patterns and autonomic measures, respectively highlighting hyperreactivity and impaired regulation.
Use concrete strategies aligned with these mechanisms: slow-paced breathing (6 breaths/min) to boost vagal tone; a 20–30 second delay before responding to allow PFC recruitment; brief grounding (name five visible objects aloud) to shift attention from interoceptive loops; and HRV biofeedback sessions twice weekly for 6–8 weeks to raise baseline regulatory capacity. Wearable technology can detect rising sympathetic markers and prompt these strategies automatically.
For clinical assessment, combine self-report scales with objective measures: continuous HRV, skin conductance, and EMG during a standardized provocation task yield quantitative indices of reactivity and regulation. Cognitive interventions should train lexical reappraisal and behavioural response inhibition, done repeatedly to strengthen PFC–amygdala connectivity. When aggression includes hitting or risk of harm, apply behavioural contingency measures and seek specialist care.
Track outcomes with simple, repeatable metrics: resting HRV, frequency of intense episodes per week, peak heart rate during provocation, and subjective anger rated 0–10. Use these measures to compare progress and adjust a personalised strategy extending from brief breathwork to longer-term therapy for severe cases.
Identifying amygdala–prefrontal signatures that forecast an anger flare
Recommendation: Monitor amygdala–prefrontal functional coupling together with cardiovascular signals and brief hormonal sampling; flag an alert when prefrontal regulation falls by ~0.15–0.25 Fisher z while systolic pressure rises ≥12–15 mmHg and heart rate increases ≥8–10 bpm, since studies revealed that combination predicts near-term anger flares with substantially higher probability.
fMRI and task-based probes from minati and harrison show exactly where coupling shifts: reduced ventromedial prefrontal (vmPFC) influence on the amygdala precedes outward anger, whereas schultheiss work links concurrent rises in catecholamine-driven hormones and sympathetic activation to faster escalation. Mechanistically, a loss of inhibitory control in prefrontal circuits permits facilitatory pathways through the periaqueductal region to engage rapid motor and autonomic outputs that support defensive action against perceived threat or fear.
Use a simple protocol for applied monitoring: record a 5-minute neutral baseline, then run a 3–5 minute threat-eliciting task or real-world sampling while capturing heart rate variability, systolic and diastolic pressure, and time-stamped saliva for cortisol when feasible. Employ lightweight software that computes a connectivity index and compares it against baseline; set thresholds so the system alerts you when amygdala–prefrontal coupling drops >0.15 z and cardiovascular rate changes exceed the values above. These combined markers predict escalation much better than any single measure alone.
Actionable steps when a signature appears: (1) stop and orient yourself for 30–60 seconds, slow breathing to a rate of ~6/min to blunt sympathetic surge, (2) deploy a focused reappraisal script that shifts attention from threat-related interpretations to concrete facts, (3) use brief behavioral counters such as stepping back physically or naming the physiological changes aloud to engage prefrontal decision-making processes. Repeat this sequence for three cycles; physiological data show systolic and hormonal responses begin to attenuate within 10–20 minutes when regulatory processes reengage.
How autonomic markers (heart rate, skin conductance) change during escalation
Monitor heart rate and skin conductance continuously and intervene when heart rate increases by more than 10–20 bpm from baseline or when skin conductance phasic amplitude exceeds 0.05–0.1 μS, because these thresholds reliably indicate escalation after a provocative stimulus; heres concise thresholds and actions to take immediately.
Baseline: resting heart rate typically sits 60–75 bpm with RMSSD (HRV) 30–50 ms and tonic skin conductance level (SCL) 2–6 μS. Orienting response (0–3 s after stimulus) produces a transient HR deceleration of 2–6 bpm then a rebound; phasic SCR latency is 1–3 s with amplitudes 0.05–0.2 μS. Escalation phase (30–120 s) shows HR increases of 10–30 bpm, HRV reduced by 20–40%, SCR frequency rising to 3–6/min, and tonic SCL increases of 0.5–2 μS–use these figure values to set real-time flags.
Peak: within 2–5 minutes autonomic load often peaks; heart rate can reach +30–45 bpm from baseline in high arousal and SCL can rise another 0.5–1 μS. Recovery begins when HR and SCL decline together; a successful regulatory shift shows HR dropping 5–15 bpm and SCL decreasing 0.2–0.8 μS within 3–10 minutes. Bipolar ECG leads capture cardiac timing reliably for HRV analysis, and simultaneous skin conductance measures separate tonic and phasic components for clearer interpretation of change.
Neural and psychological links: amygdala and insula hemodynamic signals correlate with fast increases in skin conductance and HR, since amygdala activity activates sympathetic output; dorsal medial prefrontal cortex reductions track reduced regulatory capacity. Subliminally presented threat cues and implicit facial expressions (emotional faces) produce measurable autonomic shifts even without conscious awareness, which supports using brief implicit tests in experimental psychology to estimate anger propensity and reactivity.
Practical steps to reduce escalation: apply paced breathing at 5–6 breaths/min to lower HR by 5–10 bpm within 60–90 s and reduce SCR amplitude by ~20–40%; instruct cognitive reappraisal to engage prefrontal regulatory circuits and reduce HRV loss over 2–5 minutes. Use biofeedback displays so people are ready to act when measures cross thresholds; keep interventions under 3 minutes for best compliance and expect measurable improvement in both HR and SCL within that window.
Data workflow recommendations: log heart rate, RMSSD, SCL tonic and SCR phasic timestamps, and timestamped stimuli for later analysis. When profiling individual propensity to escalate, combine autonomic time-series with behavioral markers (verbal tone, facial and facial-muscle EMG) and mental-state ratings; models that include implicit responses capture variance that self-report misses. Use these objective measures to set personalized alarms and brief regulatory prompts that should reduce peak autonomic load and speed recovery.
What adrenaline and cortisol do to cognition and impulse control in the moment
Breathe slowly for six seconds in, six seconds out before you act; this immediate step reduces adrenaline-driven reactivity and gives the frontal lobe time to resume controlled processing.
Adrenaline (epinephrine) releases within seconds from the adrenal medulla and increases heart rate, blood pressure and glucose availability; its plasma half-life is roughly 2–3 minutes, but sympathetic arousal and autonomic signs can persist longer. Cortisol, produced by the HPA axis, rises more slowly, typically peaking about 20–30 minutes after a stressor and remaining elevated for 60–90 minutes. These two hormones work differently yet together: adrenaline sharpens threat detection and creates attentional fixation on salient cues, while cortisol alters hippocampal and prefrontal processing and shifts resource allocation away from complex decision-making.
- Neural effects: increased amygdala activation and decreased firing in dorsolateral prefrontal regions reduce working memory capacity and impulse control, making destructive or reflexive responses more likely.
- Perception and behavior: stress increases the chance of interpreting ambiguous signals as threats, produces short-term analgesia (reduced pain perception), and favors fast action over deliberation.
- Evolutionary explanation: this suite of responses favored immediate survival by prioritizing rapid motor output and simple threat processing, but in modern contexts it undermines nuanced social decision-making and problem-solving.
Apply these specific, evidence-aligned tactics to preserve cognition and avoid impulsive harm:
- Delay responses to emotionally charged messages – for an angry email, wait at least 20–30 minutes before replying; delaying allows adrenaline to decline and avoids cortisol-driven memory biases.
- Use biological counters: perform 6/6 slow breathing for 2–5 minutes to activate parasympathetic tone; a brief face splash with cool water or 30 seconds of humming can engage vagal pathways as non-invasive regulation.
- Shift attention physically: step outside for a 3–10 minute walk to reduce sympathetically mediated fixation and restore frontal lobe processing.
- Name the feeling aloud: a single sentence (“I feel angry and physiologically triggered”) reduces amygdala reactivity and improves prefrontal control according to psychology studies on labeling.
- Create a buffer rule for high-stakes choices: postpone decisions that could be destructive until physiological markers normalize – typically several tens of minutes for adrenaline and hours for full cortisol recovery.
- If minor confrontations are unavoidable, set a script: short, factual statements limit emotional escalation and contribute to clearer outcomes.
When presenting options under stress, remember that different physiological timelines contribute to behavior: adrenaline produces immediate mobilization and attentional narrowing, while cortisol modifies memory and valuation over the next hour. Breathe, wait, and use simple external rules (delay, script, physical break) to convert transient arousal into non-destructive action; nevertheless, persistent or extreme responses warrant consultation with a clinician about targeted, non-invasive interventions and training in stress regulation presented by behavioral therapies.
Why sleep loss, hunger, and glucose shifts raise anger reactivity
Prioritize regular sleep and steady snacks: aim for 7–9 hours most nights and keep a small protein-plus-carb snack every 3–4 hours to cut acute anger spikes. Follow a simple rule: if you start to lose focus or feel irritable, have 10–15 g of carbohydrate plus 10–20 g of protein within 20 minutes and reassess mood.
Sleep loss and drops in circulating glucose impair top-down control and speed up limbic reactivity: reduced prefrontal inhibition and increased amygdala responses raise the likelihood of aggressive responses. Neuroimage work by Chronaki and colleagues links increased dorsal anterior cingulate engagement to sleep- and hunger-related reactivity, while other studies report higher systolic pressure during anger episodes. Experimental results show sleep deprivation amplifies emotional reactivity and low glucose reduces self-regulation, respectively, producing faster, more bodily expressions of anger.
Use brief, actionable measurements to manage risk. When instructed to take a one-minute breathing test or label feelings with words, people often cut subjective anger and lower physiological markers that were previously assessed in lab tests. Keep a mood-and-hunger log: record time since last meal, sleep hours, and a one-to-five irritation score; a figure of two missed meals or fewer than six hours of sleep predicts larger reactivity in some individuals. If you leave school or work hungry, plan a portable snack to avoid escalating responses later.
Address unmet needs before they escalate: bite-sized strategies–drink 200–300 ml water, eat a 150–200 kcal balanced snack, step outside for five minutes–reduce the chance that small metabolic shifts cause outsized anger. Train labeling (use clear words for sensations) and a two-breath pause before replying; these two steps improve control strength on subsequent tasks and show measurable results on tests of self-control.
Consider individual differences. Personality traits influence baseline reactivity, but bodily states often explain momentary spikes that people frequently hear labeled as “just their personality.” Track how sleep, hunger, and glucose affect you over two weeks and share the log with a clinician if high reactivity persists; clinicians can assess hormonal or blood-glucose causes and tailor interventions that target both brain circuits and bodily triggers.
Practical detection: using wearable sensors to catch early physiological warning signs
Start with a combined-sensor configuration: single-lead ECG (250–500 Hz), PPG (100 Hz), electrodermal activity (EDA) 4–32 Hz and a 3-axis accelerometer (50–100 Hz). Set individualized baselines over 7 nights including sleep and daytime rest, then trigger alerts when real-time metrics cross relative thresholds described below.
Set these actionable thresholds against the personal baseline: RMSSD drop ≥35% over 120 seconds; heart rate increase ≥12 bpm sustained for 30–60 seconds; EDA rise ≥0.05 μS per 10 seconds; respiratory rate increase ≥4 breaths/min; peripheral skin temperature decrease ≥0.2 °C. Calibrate blood pressure sensors to flag systolic increases ≥12 mmHg if cuffless estimates are validated. These numbers signify a moderate sympathetic surge with documented correlation to anxious episodes and anger escalation.
Place ECG patches on the sternum or left parasternal area for stable QRS amplitude; place PPG on the index or ring finger for best signal during pressure changes. Avoid strong magnetic fields and hospital-grade MRI rooms; magnetic interference and nearby ohmeda respiratory monitors can distort traces. Mark times of recent substance intake (alcohol, caffeine, nicotine, stimulants) because these substances shift baselines for 6–24 hours and magnify signal magnitude.
| Metric | Sampling | Trigger Threshold (relative) | Immediate Action |
|---|---|---|---|
| ECG RMSSD | 250–500 Hz | Drop ≥35% over 2 min | Prompt 60s paced-breathing cue; log episode |
| Heart rate | 100 Hz | Increase ≥12 bpm sustained 30–60s | Haptic alert; suggest grounding task |
| EDA | 4–32 Hz | Rise ≥0.05 μS/10s | Short mindfulness prompt; record context |
| Respiration | 25–100 Hz (capnography preferred) | Rate +4 breaths/min or irregular pattern | Guided slow-breathing audio |
| Skin temp | 1 Hz | Drop ≥0.2 °C | Check peripheral perfusion; advise warming |
Combine signals with a simple scoring rule: assign 1–3 points per threshold exceedance weighted by magnitude; trigger an intervention at ≥6 points within 3 minutes. Use adaptive sensitivity so alerts decrease during scheduled exercise or sleep. Facilitate facilitator settings (facilitatory haptics or vibration intensity) that users can tune consciously; offer options to adjust false-positive tolerance.
Pair objective detection with short self-report prompts delivered as three-letter letters codes (e.g., ANX, HRT, BRE) and a two-question context form: “Where are you?” and “Any recent substance?” Store answers alongside timestamps to improve models and inform therapy. kass-style single-case logging and sonnby-borgstrom-like aggregated episode analysis improve predictive value when teams review patterns monthly.
Design interventions that respect privacy and autonomy: local device prompts (breathing, posture change) for low-probability alerts; coach contact or therapy escalation for sustained high-probability episodes. Use explicit thresholds for escalation decisions and record the decision magnitudes to audit false alarms. Integrate alerts with behavioral-therapy exercises and allow users to accept or dismiss prompts consciously.
Monitor battery and data integrity: require at least 4 hours continuous recording per 24-hour window and sync nightly; label missing-data intervals and place logs in secure systems. Train users to charge before sleep to capture nocturnal baseline shifts and post-sleep reactivity. Use encrypted storage and clear consent about who accesses event letters and episodes.
Expect residual uncertainty: sensors reduce reaction time but do not predict intent. Calibrate algorithms per individual, review false positives weekly, and update thresholds when sleep patterns, medications or chronic conditions change. Nevertheless, combining multi-modal physiological signals with short-context queries provides a measurable means to detect early arousal and to support better decisions and targeted therapy.


 The Science of Anger – What Happens in Your Brain and Body">
The Science of Anger – What Happens in Your Brain and Body">

 Missing Someone and Mental Health – Understanding the Link">
Missing Someone and Mental Health – Understanding the Link">
 What It Means If You Don’t Trust People – Signs, Causes & How to Cope">
What It Means If You Don’t Trust People – Signs, Causes & How to Cope">
 Understanding Unrequited Love – How to Move On – A Practical Guide">
Understanding Unrequited Love – How to Move On – A Practical Guide">
 Is a Polyamorous Relationship Right for You? Signs, Pros & Tips">
Is a Polyamorous Relationship Right for You? Signs, Pros & Tips">
 Avoidant Attachment in Relationships – The Complete Guide">
Avoidant Attachment in Relationships – The Complete Guide">
 Finding Strength in Vulnerability – Embrace Openness & Authenticity">
Finding Strength in Vulnerability – Embrace Openness & Authenticity">
 Divorce After Betrayal – How to Tell Children & Next Steps">
Divorce After Betrayal – How to Tell Children & Next Steps">
 Should You Share Your Location With Your Partner? Guide">
Should You Share Your Location With Your Partner? Guide">
 How to Embrace Self-Acceptance – Practical Tips for Confidence">
How to Embrace Self-Acceptance – Practical Tips for Confidence">