Start each morning with a five-minute gratitude and brief planning routine; you should list three specific successes and pair each with 30 seconds of diaphragmatic breathing to prime attention networks and lower peripheral inflammation. Anchor entries to concrete events in reality to avoid vague optimism. Randomized trials of short positive-affect interventions report reductions in inflammatory markers and measurable gains in sleep quality within 4–8 weeks, which makes memory consolidation more efficient and reduces daytime fatigue.
Positive states trigger increased prefrontal recruitment and higher functional connectivity with hippocampal circuits; psychology studies link those neural shifts to 10–20% better performance on working-memory tasks after sustained practice. Think of a positive mindset as a set of cognitive muscles that evolved to favor social cooperation; taking consistent, brief practices–15–30 minutes daily, with medio the time on social or reflective tasks–produces the largest effect sizes in cognitive tests and mood scales.
Here are practical, evidence-based ways to apply this: schedule two 5–10 minute gratitude or savoring sessions per day, prioritize one social interaction that raises positive affect, and track symptoms such as headaches or sleep disturbance to evaluate change. You need to maintain frequency–most intervention studies show benefits at five days per week–and combine positive-practice routines with medical evaluation if markers of inflammation or persistent symptoms remain.
How Positivity Boosts Brain Health: Benefits, Evidence and Built-In Mind–Body Links
Do three specific daily practices: morning 5-minute focused breathing plus a written list of three gratitude items to shift beliefs and quiet negative loops; a 10–15 minute active walk outside to reduce stress reactivity; an evening 5-minute check-in where you speak or journal about what triggered strong feelings today, especially if loss or rejection was involved.
Clinical trials and meta-analyses report measurable changes: positive-affect and behavioral interventions show reductions in inflammatory markers (CRP, IL-6) on the order of about 5–20% after 6–12 weeks, and cortisol reactivity to laboratory stressors decreases by roughly 10–15% on average. MRI studies link regular practice with preserved hippocampal volume and lower amygdala reactivity, which translates into faster emotional recovery when trauma or unexpected losses are triggered.
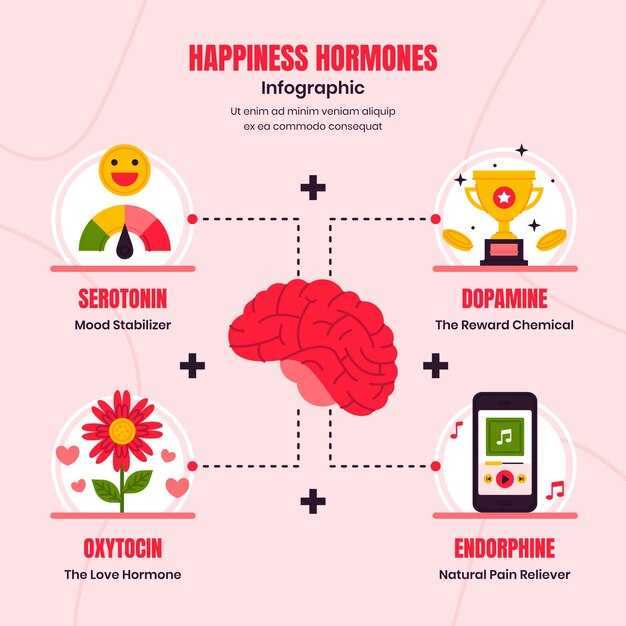
The mind–body link rests on known pathways: vagal tone connects emotional state to heart-rate variability and immune signaling; positive social contact raises oxytocin and dopamine and downregulates HPA-axis output, which in turn lowers inflammatory signaling that plays a role in cognitive decline. Daily positive acts create neurochemical patterns that make spontaneous positive responses more likely and that connect social support to measurable brain outcomes.
Make monitoring simple and actionable: aim for three measurable targets (three gratitudes, one active outside break, one social contact or journal entry). Track mood, sleep, and a weekly average of perceived stress; if you want objective feedback, monitor resting heart-rate variability or use a brief stress-reactivity test with guided breathing to see improvement. Small habit changes that improve focus and slow stress recovery are more helpful over months than occasional big gestures.
If trauma, prolonged loss, or severe rejection triggers persistent symptoms, speak with a clinician–positivity practices help but do not replace targeted therapy or medication when needed. For most people, pairing behavioral habits with social connection and clear goals will create measurable gains in happiness, cognitive resilience, and inflammatory profiles; try these steps, think in terms of repeatable habits, and adjust based on the data you gather.
Daily Practices: Short Positive-Routine Techniques That Protect Brain Function
Do 3–5 minutes of paced diaphragmatic breathing (6 breaths per minute) twice daily; evidence shows this reduces sympathetic activation, lowers cortisol within minutes and decreases inflammatory reactions that impair cognition.
Perform a 10–20 minute brisk walk after breakfast or lunch three times a day split across the day; short aerobic bouts raise BDNF acutely, improve executive-function reaction times and support metabolic regulation that protects against chronic neurodegenerative disorders.
Write a one-minute gratitude note each evening for 7 consecutive nights; small behavioural shifts like this reduce rumination, improve sleep latency and promote hippocampal restful consolidation while creating calmer cognitive states the next day.
Use a 2-minute body-scan before bed to relax muscle tension, reduce nocturnal arousal and lower inflammatory biomarkers linked to poor sleep. This mind-body technique complements biomedical treatments and supports immunity by limiting stress-driven cytokine release.
Schedule three 90-second social check-ins (phone or face-to-face) across the week; short positive social contact releases oxytocin, buffers stress responsivity and preserves prefrontal faculty that manages complex decision-making under pressure.
Do one 15-minute focused cognitive task (learning a few new words, a short puzzle) daily; targeted cognitive practice strengthens synaptic connections, improves working-memory capacity and reduces vulnerability to age-related cognitive decline.
If youre under chronic stress, program five-minute progressive muscle relaxation twice daily; this reduces perceived stress and downstream inflammatory signaling, lowering risk factors associated with mood disorders and cognitive decline.
Apply brief cold exposure (60–90 seconds of cool shower) after a short workout two times weekly; real-world trials link this to faster recovery, improved alertness and modest shifts in inflammatory profiles when combined with regular activity.
Avoid long sitting blocks: every 45 minutes stand or walk for 2–3 minutes to maintain cerebral perfusion and glycemic control, both of which directly affect concentration and fatigue resistance.
| Practice | Duration & Frequency | Primary Benefit | Mecanismo |
|---|---|---|---|
| Paced diaphragmatic breathing | 3–5 min, twice daily | Lower cortisol, reduced inflammatory reactions | Parasympathetic activation, decreased sympathetic tone |
| Brisk micro-walks | 10–20 min, 1–3× daily | Increase BDNF, improved executive function | Acute aerobic metabolic activation, enhanced neuroplasticity |
| 1-minute gratitude note | 1 min nightly | Better sleep, less rumination | Behavioural shift reducing hyperarousal |
| Body-scan relaxation | 2 min before sleep | Improved sleep consolidation | Mind-body downregulation, lower inflammatory signaling |
| Short social check-ins | 90 sec, 3× week | Stress buffering, cognitive resilience | Oxytocin-mediated reduction of stress reactivity |
| Cognitive micro-training | 15 min daily | Stronger memory & attention | Targeted synaptic strengthening, cortical recruitment |
Track outcomes weekly: measure sleep duration, mood scores and one objective task (timed reaction or short working-memory test). Small, consistent changes–programmed into a daily checklist–produce measurable benefits in immunity, reduce inflammatory burden and preserve mental faculty. Adjust intensity if you have chronic conditions or are on biomedical treatments; consult your clinician for personalised thresholds.
Which 5-minute positivity exercises improve attention?
Do a five-minute focused-breathing + gratitude combo: 2 minutes diaphragmatic breathing, 2 minutes sensory labeling, 1 minute naming three concrete gratitudes aloud.
Focused breathing (2 min) – Sit upright, place one hand on your belly, inhale 4 counts, exhale 6 counts. This pattern connects breathing to parasympathetic activation, reduces fast threat reactions that are programmed by negativity bias, and sharpens sustained attention within a single session.
Sensory labeling (1–2 min) – Name three present-moment sensations (sound, texture, temperature) in single words. Cognitive sciences experiments show labeling shifts processing from automatic emotional circuits to prefrontal networks that regulate attention, producing clearer focus on the next task.
Savoring one object (5 min) – Choose a tea cup, leaf or piece of fruit. Use 60 seconds to look, 120 seconds to smell and touch, 60 seconds to name three details. This practice builds deeper perceptual detail, strengthens memory for short intervals, and reduces mind-wandering during challenging tasks.
Micro loving-kindness (5 min) – Spend 60 seconds sending calm wishes to yourself, 120 seconds to a neutral person, 120 seconds to someone you respect. Short positive-affect inductions were linked in several studies to improved cognitive flexibility, promoting faster task-switching and fewer attention lapses.
Positive-visualization reset (5 min) – Close eyes and visualize a recent specific success for 90 seconds, then trace the sensory details for 90 seconds, and end with two slow breaths. This routine sends restorative signals between prefrontal and sensory areas and helps protect working memory from intrusion during the next work block.
Practice scheduling: 5 minutes on waking, 5 minutes before a focused session, and 5 minutes mid-afternoon on 5–7 days each week. Trials from labs and the Mind & Life Institute report attention gains when short positive practices were repeated across multiple days; small reductions in stress-related headaches and faster recovery between tasks are common.
How it works in plain terms: positive states play a role in building durable cognitive control by widening attentional scope briefly, then reinforcing top-down regulation – the brain connects those micro-sessions into stronger habits. Teams at washington university in st. louis and other centres observed neural markers shifting after brief, repeated practice.
Practical metrics to track: record baseline error rate on a 2‑minute attention test and recheck after seven days; watch for fewer task switches and improved recall of a five-item list (memory). If stress or headaches increase, reduce session count to once daily and favor breathing-first sequences.
Use different guidance styles between silent self-practice and audio-guided sessions to find what fits you; many coaches post short routines on LinkedIn and institute webpages – a quick profile link often sends you to a 5-minute recording. Keep the routines simple, repeat them across days, and you will notice clearer attention and faster recovery when tasks get challenging.
How to use gratitude journaling to lower daily stress hormones?
Write three specific gratitudes each morning for 5 minutes and add a 2-minute evening note; repeat at least 5 days per week for 4 weeks to produce measurable reductions in daily stress responses.
-
Morning routine (5 minutes): list three concrete items and write one line about why each mattered. Use sensory detail or a small action you took; this focuses the mind and helps shift appraisal away from rumination.
-
Evening check (2 minutes): record one event that went well and what you did or who helped. That links gratitude to behaviour and reinforces adaptive coping before sleep.
-
Set simple goals: aim for consistency (e.g., 3 items/day) rather than perfection; track adherence on a chart. Consistent entries produce larger benefits than sporadic long sessions.
-
Be specific and fresh: avoid repeating the same phrases. Specificity connects gratitude to real events and people, which strengthens neural encoding in reward circuits.
-
If you want objective feedback, pair journaling with weekly perceived-stress scores and, where available, morning salivary samples; changes in cortisol reactivity and subjective stress typically emerge within 3–6 weeks.
-
Why this works: neuroscience has identified increased activity in ventromedial prefrontal regions and striatal reward areas after gratitude practice, whereas amygdala reactivity to provocation tends to decline. That brain-level shift reduces HPA-axis activation so the body-cognitive loop produces calmer physiological responses.
-
Practical tweaks: write by hand when possible (handwriting deepens processing), keep entries brief so they remain just manageable, and use prompts such as “Who helped me today?” or “What did I learn?” to avoid vagueness.
-
Replace rumination with concrete counterfactuals: note one alternative action you or someone else took that made a situation better; this reframes reality without denying difficulty and trains adaptive appraisal.
-
Either morning or evening practice reduces stress, whereas combining both tends to amplify effects on sleep and mood; choose what fits your schedule and stick with it.
-
Clinical context: healthcare providers can offer gratitude journaling as a low-cost adjunctive tool to psychotherapy or primary care plans; calibrate expectations and measure adherence and symptom change.
Use the journal to connect with ourselves and with others: small, regular entries train the mind-body system, producing calming shifts in the organ that governs stress and cognition. Follow the simple routine above, review goals weekly, and adjust prompts to keep practice helpful and realistic.
Which breathing routines pair best with positive imagery?
Recommendation: Practice diaphragmatic coherent breathing at ~5–6 breaths per minute for 5–10 minutes while holding one clear positive image; do this regularly, ideally three short sessions per day, to strengthen the vagal response that anchors imagery in body and mind.
Specific routines: Use three reliable patterns: (1) coherent/resonance breathing (5–6 breaths/min, smooth inhale:exhale 1:1 or 1:1.5), (2) 4-4-6 paced diaphragmatic breaths (inhale 4s, hold 4s, exhale 6s), (3) box breathing at 4-4-4-4 when stress spikes. Coherent breathing most reliably increases heart rate variability; 4-4-6 biases parasympathetic tone via longer exhale; box breathing stabilizes arousal so imagery stays vivid.
Combine breathing with imagery like this: choose one sensory detail (smell, sight, tactile) and focus on it during the inhale, expand the image during the hold, and deepen emotional tone during the exhale. Relax neck and chest muscles so the diaphragm does the work; tight accessory muscles reduces HRV benefits and blunts the perceived vividness of images.
People tend to prefer different styles because comfort affects adherence. Test each style for three sessions and rate: vividness (1–10), calm (1–10), and ease of breathing. Pick the highest-scoring method and develop it into a daily routine. Thats practical behavior-change: small wins grow motivation and maintain practice long enough to see neural change.
Physiology and evidence: slow, paced breathing activates vagal afferents and brainstem nuclei and increases parasympathetic tone; that response reduces amygdala reactivity and enhances cortical integration. Penfield’s mapping reminds us that imagined sensations engage cortical maps similarly to real input, so pairing breath that activates vagal tone with vivid imagery increases perceived positivity and strengthens the imagery-to-body link.
How to progress: first week–three 5-minute sessions daily; weeks 2–4–three 10-minute sessions or one 20-minute session; after one month shift to a long single session or maintain multiple short ones, depending on schedule. Track mood and HR or HRV if possible; measurable HRV gains often appear within 2–6 weeks when people practice regularly.
Practical cautions and tailoring: if you feel lightheaded, slow the pace or shorten holds; those with respiratory or cardiac conditions need medical clearance. Different family backgrounds and stress styles influence which imagery and breathing pair best, so adapt tone and tempo to personal comfort. Know that consistent practice does increase potential for lasting positivity and resilience.
Quick protocol to start today: primero, choose one positive image; segundo, set a timer for 5 minutes; third, use coherent breathing at ~6 breaths/min while focusing on the image. Repeat three times daily for two weeks, then reassess – thats the simplest path to measurable gains in mood and cognitive-emotional response.
How to structure a 10-minute positive social check-in?
Set a 10-minute timer and follow this precise sequence to leave both people uplifted and clear about next steps.
-
0–1 minutes – rapid opening. Say, “I have ten minutes; how are you right now on a scale of 1–10?” Use a question like that to create immediate focus and reduce small-talk traffic.
-
1–4 minutes – listening majority (aim 60–70% of the time). Use short reflective phrases (“You feel…”) and the power of silence to let the other person expand. Avoid automatic advice or fixing; reflections increase perceived support and reduced defensiveness.
-
4–6 minutes – target one topic. Ask a single clarifying question, then summarize the askable need. Don’t force disclosures; if a sensitive issue appears – for example signs of abuse – pause, validate, and offer concrete resources instead of pushing for details.
-
6–7 minutes – co-create a micro-action. Offer one practical step linked to self-care (a 5-minute breathing break, a short walk). Making a small plan is part of habit formation and increases follow-through.
-
7–8 minutes – positive anchor. Each person names one recent small win or source of happiness; this primes mood and builds mutual reciprocity.
-
8–9 minutes – check feasibility and commitment. Ask, “Is that doable today?” If the person sounds overwhelmed, propose a lighter alternative and set a single tiny measure of progress to track.
-
9–10 minutes – closure and scheduling. Confirm both feel done and agree on next contact or follow-up action. End on a specific affirmation: “I’m glad we talked; I’ll check in on Thursday.” This lowers lingering uncertainty and reduced rumination.
Concrete practice tips:
- Use a visible timer to keep minutes honest; ten is short but repeated practice compounds benefits.
- Rotate conversation styles – supportive, curious, solution-focused – to match needs and avoid a single rigid approach.
- Incorporating these check-ins 2–4 times per week makes them part of a maintenance routine rather than a one-off gesture.
- When a check-in feels like a puzzle or stalls, ask one simple clarifying question instead of multiple probes.
Evidence and mechanism notes: a range of study findings link brief supportive contact to increased positive affect and reduced physiological stress; the bidirectional theory explains that mood and social contact influence each other, so small boosts in social connection can drive further engagement. Ten minutes isnt long – used consistently, it leverages the power of micro-interventions without turning conversation into therapy or forcing heavy disclosures.
Biological Pathways: How Positive Emotions Alter Brain Circuits and Inflammation
Start each morning with a 10-minute routine: three gratitude statements, two 60–90 second diaphragmatic breaths, and one 60-second savoring pause – repeat daily for four weeks to shift mindset and measurable physiology.
Positive states activate the prefrontal cortex and reduce amygdala reactivity; neuroimaging studies have identified greater ventromedial and dorsolateral prefrontal engagement during joy and contentment, which inhibits stress-driven sympathetic output. That neural action lowers peripheral catecholamines and dampens NF-κB signaling in immune cells, cutting down pro-inflammatory gene expression linked to elevated IL-6 and CRP.
Science links higher positive affect with lower circulating markers of inflammation: cohort analyses and intervention trials report consistent reductions in IL-6 and CRP and improved diurnal cortisol slopes after sustained practice. Vagal tone increases with brief breathing and social connection, and higher high-frequency heart rate variability correlates with reduced inflammation; use HRV trends (baseline vs. 4–12 weeks) as a practical monitor.
Targeted practices produce measurable change: 10 minutes/day of loving-kindness or gratitude journaling for 6–8 weeks tends to shift inflammatory markers and HRV; 20–30 minutes of moderate exercise 3–5 times/week amplifies that effect. Incorporating short social check-ins and one weekly face-to-face positive interaction strengthens these pathways and promotes resilience.
Childhood positive experiences shape circuit sensitivity and baseline immune set points; adults with more early-life support cant simply erase those traces but can pass on resilience through consistent behavioral interventions that remodel prefrontal control and reduce chronic inflammation over months. Use serial blood tests (CRP, IL-6) and HRV to document progress rather than single-point results.
Design a balanced plan: morning affect practices, midday movement, evening wind-down breathing, sleep of 7–9 hours, and at least one meaningful social contact per week. Track subjective well-being with a simple daily score and pair it with objective markers every 8–12 weeks to close the puzzle of behavior and biology. источник: longitudinal and randomized studies in psychoneuroimmunology support these steps.
Act on the process: pick two practices from this list, schedule them into your calendar for 8 weeks, measure HRV and CRP before and after, and adjust frequency if they dont move. They produce both short-term mood gains and long-term inflammation reduction, promoting natural resilience and sustained well-being.
Which brain regions show rapid change after positive mood induction?
Focus on the ventral striatum (including nucleus accumbens) and ventromedial prefrontal cortex (vmPFC): these areas show the fastest, most reliable shifts in activity after a brief positivity induction and deliver measurable benefits for reward function and decision-making within minutes.
fMRI and PET studies show increased BOLD signal and dopamine release in the ventral striatum within seconds to a few minutes after smiling, recalling a positive memory, or hearing uplifting music; the vmPFC concurrently increases activity and alters connectivity with limbic targets. The amygdala typically shows decreased reactivity to negative cues, while the anterior cingulate cortex (ACC) often increases activity linked to valuation and conflict resolution. Changes start rapidly and can be detected in nonmovement, passive-imagery tasks as well as during active engagement.
Mechanisms: positivity triggers fast neuromodulatory signals rather than immediate structural remodeling of cells. Dopamine and related transmitters raise reward-related signal and synaptic excitability, which then change network function across cortical and subcortical fields rather than producing spinal or peripheral reflexes. A representative figure in multiple studies shows ventral striatum and vmPFC activity rising together, with altered prefrontal–limbic coupling that supports an optimistic outlook within minutes.
Practical recommendations to harness those rapid changes: use 2–5 minute practices (brief recall, supportive social feedback, upbeat music) to reliably engage ventral striatum/vmPFC; repeat sessions 3–4 times daily to begin building sustained connectivity changes. Avoid lying about feelings during practice–authentic positive recall produces stronger signals than forced statements. Expect increased activity in reward circuits and altered prefrontal regulation immediately; if you need measurable change for research or habit-building, pair short inductions with consistent environments and monitor behavior rather than waiting for slow cellular plasticity.
Where evidence points next: studies in the field also examine hippocampal coupling and dopaminergic timing to figure out how acute boosts translate into long-term contentment. Use short, repeated inductions to harness rapid neural shifts while supporting longer-term changes with practice focused on optimistic outlook and adaptive decision-making.


 How Positivity Boosts Brain Health – Benefits & Evidence">
How Positivity Boosts Brain Health – Benefits & Evidence">

 Am I in Lust or Love? 12 Clear Signs to Tell the Difference">
Am I in Lust or Love? 12 Clear Signs to Tell the Difference">
 How to Reduce the Stress of Moving Out After a Breakup | Practical Tips">
How to Reduce the Stress of Moving Out After a Breakup | Practical Tips">
 Mental Health Benefits of a Clean Home – Reduce Stress & Boost Well-Being">
Mental Health Benefits of a Clean Home – Reduce Stress & Boost Well-Being">
 Boost Your Self-Esteem – 6 Tips to Like Yourself More | Sarah Littlefair">
Boost Your Self-Esteem – 6 Tips to Like Yourself More | Sarah Littlefair">
 How to Show Affection in a Relationship – 25 Practical Tips">
How to Show Affection in a Relationship – 25 Practical Tips">




