Record day 1 (first bleed), flow, basal body temperature, cervical mucus, and daily symptoms for at least three cycles; theres clear physiology behind each phase and that record will guide specific changes. Map typical ranges (menstruation ~ days 1–5, follicular ~ 6–14, ovulation around day 14, luteal ~ 15–28) and use those dates to time calories, macros, supplements, and training.
Nutrition targets by phase: during follicular/ovulation increase carbohydrates to roughly 45–55% of calories, aim for 20–30 g protein per meal and prioritize complex carbs to support strength and endurance sessions. In luteal lower carbs to about 35–45% and raise fats to 30–40% – include fatty fish and grass-fed options for omega-3 and fat-soluble nutrients. Add iron-ritch (ritch) foods like grass-fed liver, spinach, and lentils on heavier-bleed days, and target 25–35 g fiber daily to regulate bloating.
Exercise guidance: schedule higher-load strength work and longer endurance intervals in the high-energy window (follicular + ovulation). Shift toward pilates, mobility, and lower-intensity endurance in the luteal and menstrual windows to manage inflammation and conserve energy. If you plan longer sessions, consume 30–60 g carbohydrates 60–90 minutes before and add 20–40 g protein after to speed recovery and reduce fatigue.
Symptom tactics: consider 200–400 mg magnesium at night for cramps and sleep, 1–2 g combined EPA/DHA if inflammation is a problem, and check ferritin if bleeding is heavy. Use medicine and lab support to rule out anemia, thyroid issues, or other drivers; build a small clinical and coaching support plan so adjustments don’t lead to underfueling. Many people who were consistent with these tweaks report fewer severe symptoms within two to three cycles.
Avoid the hype of one-size-fits-all protocols and focus on aligning measurable inputs with outcomes: adjust calories, tweak macros, and time workouts, then log symptoms and performance so data lead your next move. This article lays out actionable steps to help you manage cycles more predictably, feel more balanced, and train smarter for longer.
Follicular Phase (Days 6–14): Practical adjustments for tracking, activity, and symptom relief

Begin daily tracking on Day 6: record basal body temperature (BBT) each morning before rising, note cervical mucus quality, log a 0–10 energy/feeling score, and set a phone bell reminder for consistency.
Read BBT shifts as concrete signs: a sustained rise of ~0.3–0.5°C across three measurements usually marks the ovulatory transition; cervical mucus that becomes clear and stretchy signals peak fertility and the best interval to try to conceive. Clinicians often say that combining mucus and BBT improves accuracy.
Implement activity adjustments to match rising estrogen and energy. Increase resistance work: schedule 3 sessions per week of 20–40 minute strength or interval workouts (6–10 short intervals of 30–60 seconds effort with 60–90 seconds rest). Use this phase’s advantage to lift heavier, push tempo runs, or add plyometrics–these things typically feel easier now.
Address common symptoms and cramps with specific measures. Apply localized heat for 10–20 minutes, take 200–400 mg magnesium at bedtime if tolerated, and practice a daily 10-minute mobility routine for lower back and hips. For persistent problems, track severity and bring precise data to your clinician so they know patterns instead of vague complaints.
Nutrition and supplements: increase protein to ~1.2–1.6 g/kg body weight across the day to support rebuilding; include 200–300 calories post-workout; check vitamin D status and supplement if levels are low–many people commonly need correction. Add iron-rich meals if heavy bleeding earlier reduced stores; include vitamin C with iron to improve absorption.
Hormone and fertility focus: this is the ovulatory ramp-up–optimizing sleep (7–9 hours), reducing alcohol, and supporting consistent nutrient intake raises the chance to conceive during the fertile window. Track intervals between menstrual cycles to spot shorter or longer follicular phases and adjust attempts accordingly.
Mental health and healing: schedule one social or creative activity per week that feels positive and empowering, and use short breathwork when anxiety rises. Follow credible accounts for visual mucus charts on Instagram to find examples, but validate with your own data rather than relying solely on images.
| Days | Track | Activity | Symptom relief & lifestyle |
|---|---|---|---|
| 6–9 | Daily BBT, mucus notes, energy score | 2 strength sessions (20–30 min), 1 mobility session | Magnesium 200 mg nightly, heat for mild cramps, prioritize sleep |
| 10–14 | Continue BBT, watch for mucus change indicating ovulatory peak | 3 sessions: strength + one interval session (20–30 min) | Increase protein post-workout, set bell reminders for intercourse if trying to conceive, gentle core activation for lower-back relief |
Next steps: review two full cycles of your data, find patterns, and implement one small change each cycle–such as adding an extra strength day or adjusting magnesium timing–to build supporting habits without overwhelm.
Detect follicular-phase markers: basal body temperature, cervical mucus, and calendar cues
Measure basal body temperature every morning with a digital basal thermometer (0.01°C resolution) immediately upon waking and before any activity; record values for at least three cycles to establish a personal baseline and consider using a spreadsheet or reliable app to spot patterns.
In the follicular phase BBT stays lower; expect a sustained post-ovulatory rise of about 0.2–0.5°C (0.36–0.9°F) that persists for three consecutive days. If your temperature doesnt rise by that amount after a suspected fertile window, consider an LH urine test or consult a clinician because ovulation may not have occurred.
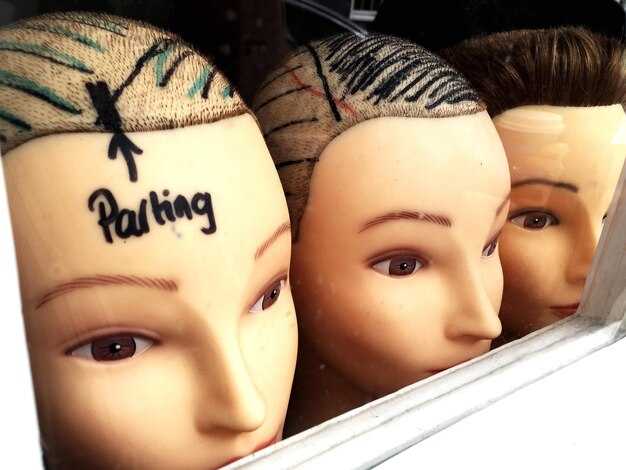
Track cervical mucus daily: early follicular mucus is scant or sticky, then increases to wet, clear and stretchy–“egg-white” mucus–within 1–3 days before ovulation. Log texture, amount and color (dry, sticky, creamy, clear/stretchy); these objective notes help distinguish natural fertile signals from nonspecific discharge and improve predictability.
Use calendar cues pragmatically: mark day 1 as first day of full flow; calculate expected ovulation by subtracting a consistent luteal length (commonly ~14 days) from your next period date. Certain cycles vary widely, so treat calendar estimates as provisional and combine them with BBT and mucus for accuracy.
For diagnostic purposes have mid-luteal serum progesterone measured ~7 days after the suspected ovulation; a blood value >3 ng/mL is commonly used to confirm ovulation. If clinical confirmation is needed, have results evaluated alongside cycle tracking data.
Prevent false readings by following strict practices: sleep at least 3–4 hours before measurement, avoid alcohol the night before, use the same thermometer and same measurement site, and minimize environmental exposure to cold or heat. Small behaviors like moving in bed or eating before recording can shift readings and reduce effectiveness.
Combine methods for stronger signals: use daily mucus notes plus BBT and targeted LH tests during suspected fertile days. Reviewed studies show that combined symptom-temperature approaches outperform single-method tracking; ignore unverified charts on pinterest and the marketing hype around one-size-fits-all apps.
Address lifestyle factors that affect markers and comfort: if you feel fatigued after menses, check blood ferritin and iron because low iron lowers energy and can skew perceived symptoms; adjust food intake (balanced protein + complex carbs) and light exercise to support metabolism. Hormone-driven brain and metabolic changes mean energy often increases in late follicular phase, so match rest and practices to how you actually feel.
Keep entries simple and consistent: use short daily notes (time, BBT, mucus category, sleep quality) for analytical purposes; consistent data across these sources makes detecting the follicular phase more effective and prevents misinterpretation of single anomalous readings.
Plan peak-focus work and social tasks around rising energy and mood
Schedule your hardest cognitive work and important social commitments in the late follicular-to-ovulatory window–about 48–72 hours before ovulation through the 24 hours after ovulation–so you use the estrogen-driven rise in energy and mood before progesterone begins to shift performance. Block 90–120 minute focus sessions in the morning hours (09:00–12:00) for the highest sustained attention, and reserve late-afternoon slots for stimulating meetings or networking when mood stays elevated.
Move presentations, negotiations and public speaking to those days; Cassandra, a product manager, shifted key client calls into that window and found the conversations were clearer and follow-ups easier to handle. Track outcomes across two cycles: log task completion, perceived focus (1–10) and number of interruptions to measure improvement from scheduling changes rather than relying on hype.
Eat for steady cognition: 1 cup blueberries with 150 g Greek yogurt plus a small handful of nuts 60–90 minutes before a focus block provides antioxidants and sustained glucose; add a 15–20 g protein source if you need longer concentration. Do gentle mobility or 20–30 minute workouts before meetings to boost alertness without creating fatigue, and avoid heavy meals right before high-focus hours.
If your cycle is irregular or you suspect a hormone issue, consider using ovulation test strips or a basal body temperature app as an objective tool, and speak with a gynecologist about patterns that were repeatedly disruptive. For people dealing with PMS symptoms later in the cycle, schedule lower-stakes, collaborative work then and save high-demand tasks for the higher-energy window.
Practical rules: always protect two uninterrupted focus blocks per peak day, leave a 60–90 minute buffer between high-stakes meetings, and use a simple checklist to start each block (task, desired outcome, 2-minute prep). Track how your bodys responses change over three cycles and adjust–small shifts in timing often yield better sustained productivity and less stress overall.
Exercise choices by day: strength, HIIT, or light cardio and how to schedule them
Prioritize strength work during your follicular and ovulatory windows, schedule HIIT for one or two peak-energy days, and choose light cardio or pilates when youre fatigued.
- Menstrual phase (days 1–4): keep intensity low to moderate. Aim for 20–40 minutes of brisk walking, gentle cycling, or a 30–45 minute pilates session. If cramps or heavy bleeding limit activity, reduce duration and focus on mobility and breath work. Short strength sessions that include 2 sets of 8–12 reps of whole-body machines or bodyweight moves work well here.
- Early follicular (days 5–9): energy rises; lead with compound lifts. Do 3 strength sessions across this window: 3–5 sets of 4–8 reps for heavy lifts (or RPE 7–8) plus one steady-state cardio session (30–45 minutes). Studies show rising estrogen improves recovery and power, so progressive overload pays off here.
- Late follicular → ovulation (days 10–16): schedule HIIT and power sessions. Two short HIITs (10–20 minutes of intervals, e.g., 30s sprint/90s rest) and 2 strength sessions focused on speed and power (3–4 sets of 3–6 explosive reps). Expect a temporary positive impact on peak strength and libido; keep recovery days after HIIT to limit soreness.
- Luteal phase (days 17–28): shift volume down and include more steady cardio. Do 2 moderate strength sessions (3 sets of 8–12 reps at RPE 6–7), 2 low-intensity cardio sessions (30–50 minutes), and a restorative class like pilates or yoga. Progesterone can increase body temperature and perceived effort, so reduce max loads if youre fatigued.
Practical scheduling for a 28-day cycle includes four targeted blocks: strength-focused weeks in follicular/ovulation, conditioning-light weeks in luteal/menstrual. Example: Week 1 (menstrual): mobility + light cardio; Week 2 (follicular): strength x3; Week 3 (ovulation): strength x2 + HIIT x1; Week 4 (luteal): mixed moderate strength + longer low-intensity cardio.
- Sets, reps and intensity guidance: prioritize progressive overload when energy allows; use RPE to adjust daily–RPE 7–8 for heavy strength, RPE 8–9 for HIIT bursts, RPE 3–5 for recovery days. Track performance so you can be evaluated against your previous cycles.
- Frequency: aim for 3–5 training days per week with 1–2 high-intensity sessions total; reduce HIIT frequency if sleep, anxiety, or cravings increase.
- Nutrition and fuel: pre-workout snacks that include carbohydrate + protein (banana + yogurt, whole-grain toast + egg) help during high-intensity days; use your grocery list to keep portable options. After tough sessions, prioritize 20–30 g protein to support recovery.
- Symptom management: if anxiety or fatigue spikes, swap a HIIT for a brisk walk or pilates class. Regular movement helps lower long-term disease risk and improves mood, but always scale to whats sustainable for you that cycle.
- Monitoring: keep a simple log of energy, sleep, cramps, cravings and performance. Speaking with a coach or clinician can help interpret patterns–many women report consistent experiences across cycles when evaluated over several months.
Small rules that make this practical: 1) schedule HIIT only on days you slept well and have low stress; 2) lead strength sessions with compound lifts and follow with 5–10 minutes of mobility; 3) limit heavy loading during heavy bleeding; 4) if cravings spike in luteal days, increase protein and fiber to reduce overeating. источник: aggregated trial data and cohort reports show these adjustments produce positive changes in energy, strength and recovery.
Nutrition and meal timing to support follicle growth and steady blood sugar
Eat 25–30 g protein and 10–15 g fiber within 30–60 minutes of waking to stabilize your blood sugar and support follicle growth.
Begin the follicular window (day 1–14) with breakfasts that combine 30 g protein, 30–40 g low‑GI carbs and 10–15 g healthy fat; follicle selection occurs during this phase and better glucose control supports regular selection.
Pair carbohydrates with protein and fat at every meal: aim for 20–40 g protein, 20–40 g complex carbs, and a tablespoon of fat per meal. That ratio slows absorption, reduces insulin spikes and leads to steadier energy rather than sharp highs and crashes down the day.
Schedule meals every 3–4 hours and include a 150–250 kcal snack if more than 4 hours separate meals; this timing helps most people avoid midafternoon dips and evening overeating. For workouts, consume 15–25 g carbs plus 10–20 g protein within 30–60 minutes after exercise to refill glycogen and support recovery.
Choose grocery items that deliver sustained nutrients: oats, lentils, canned salmon, eggs, plain Greek yogurt, leafy greens, sweet potato, avocado and almonds. Almonds are a источник of magnesium and healthy fat and make a helpful, portable snack.
Ignore one‑size‑fits‑all hype about extreme fasting or zero‑carb plans during the follicular phase; such approaches can worsen blood sugar variability and, for those struggling with infertility or irregular cycles, contribute to ovulatory disruption. Weight loss isnt the immediate goal when working to optimize ovulation–prioritize consistent intake and nutrient density first.
When cramps or bloating occur, lean toward gentle carbohydrate increases paired with protein and anti‑inflammatory fats rather than more sugar, because this reduces prostaglandin triggers and often improves symptoms within a cycle.
Practical steps to implement: prep three balanced meals and two snacks each week, list grocery staples that match the meal plan, plan workouts in the follicular window when insulin sensitivity tends to be higher, and track small improvements in sleep, mood and cycle regularity. Try these ways in this order and adjust based on your experience; small, steady changes produce larger improvements than dramatic shifts leading to burnout.
Which labs to order and when to trial supplements or herbs during days 6–14
Order these labs: baseline reproductive panel (FSH, LH, estradiol on cycle day 3), AMH (any time), TSH and free T4, prolactin, CBC, CMP (electrolytes, liver, kidney), fasting glucose and fasting insulin, 25‑OH vitamin D, ferritin, B12, iron studies, CRP, DHEA‑S and total testosterone when PCOS or androgen signs exist. Target ranges to discuss with your clinician: day‑3 FSH <10 iul, amh>1.0 ng/mL (age‑dependent), TSH roughly 0.5–2.5 mIU/L, ferritin >50 ng/mL for reproducible ovulation, 25‑OH vitamin D >30–40 ng/mL, fasting insulin <10 µIU/mL for lower insulin resistance risk.
Timing during days 6–14: get a pelvic ultrasound for follicle tracking between days 10–14 if fertility evaluation is active. Begin daily LH urine testing around day 10 until you detect a surge; check mid‑follicular estradiol only if your provider is monitoring ovarian response. Repeat ferritin and vitamin D after 8–12 weeks of supplementation. If infertility testing is indicated, add partner semen analysis and consider hysterosalpingogram or saline sonogram per your clinician.
Which supplements and herbs to trial on days 6–14 and dosing:
- Magnesium (glycinate or citrate) 200–400 mg nightly to reduce cramping and support sleep; take starting day 6 and continue through ovulation and the luteal phase if it helps your symptoms. Pair with magnesium-rich foods like pumpkin seeds, chia, sunflower seeds and a small amount of dark chocolate for extra benefit.
- Omega‑3 (EPA/DHA) 1,000–2,000 mg daily to lower inflammation and cramping; begin day 6 and take every day throughout the cycle for steady anti‑inflammatory effect.
- Vitamin D 1,000–4,000 IU daily if 25‑OH D is low; recheck level after 8–12 weeks and adjust to keep it >30–40 ng/mL.
- Iron (ferrous sulfate 65 mg elemental iron or equivalent) only if ferritin is low; aim to raise ferritin above 50 ng/mL for better ovulatory comfort and energy. Start on day 6 if deficiency confirmed, and monitor CBC/ferritin 8–12 weeks later.
- N‑acetylcysteine (NAC) 600 mg twice daily has evidence for improving ovulation in PCOS. Begin day 6 and continue through ovulation for cycles when insulin resistance or PCOS is present; discuss with your clinician if taking other medications.
- Seed cycling (food‑based approach): consume about 1 tablespoon ground pumpkin + 1 tablespoon ground flax or chia daily during days 6–14 to support follicular‑phase hormone patterns, then switch seeds in the luteal phase per your chosen protocol. Keep intake slightly higher in whole‑food form rather than processed seed bars.
- Avoid starting strong hormone‑modulating herbs (high‑dose vitex, dong quai, wild yam) during this window without clinical guidance–some herbs alter ovulation timing and can interfere with infertility treatment.
How long to trial and how to track effect: test supplements for one full cycle as an initial trial and reassess symptoms and labs after 2–3 cycles if you seek fertility improvements. Use daily symptom tracking and ovulation tracking (LH tests, basal temperature, or ultrasound when available). Note whether you feel more energized, less cramping, improved comfort, or fewer PMS symptoms – document changes for yourself so you can speak openly with your clinician.
Lifestyle pairing and cautions: prioritize whole foods and reduce processed snacks that increase inflammation; combine supplements with consistent sleep, moderate exercising, and stress management for additive benefits. Seed and food suggestions include pumpkin, chia and sunflower seeds and a small amount of dark chocolate as magnesium‑rich snacks. If you see new or worsening symptoms, signs of pregnancy, or are actively pursuing infertility care, stop herbs that affect hormones and consult your provider before continuing. Don’t rely solely on pinterest tips; use labs and clinical guidance to tune syncing choices to your endocrine system and life goals.


 Cycle Syncing – How to Understand Your Menstrual Cycle & Reduce Period Symptoms">
Cycle Syncing – How to Understand Your Menstrual Cycle & Reduce Period Symptoms">

 Short-Term Relationship Breakup – Why It Hurts & How to Heal">
Short-Term Relationship Breakup – Why It Hurts & How to Heal">
 Is He Interested? Decoding the Signs of Romantic Interest">
Is He Interested? Decoding the Signs of Romantic Interest">
 What Is the Point of Life? Why You Might Feel This Way and How to Find Meaning">
What Is the Point of Life? Why You Might Feel This Way and How to Find Meaning">
 The Importance of Family Love – Strengthening Bonds & Wellbeing">
The Importance of Family Love – Strengthening Bonds & Wellbeing">
 I Don’t Know Who I Am — How to Reconnect with Your True Self & Discover What You Want">
I Don’t Know Who I Am — How to Reconnect with Your True Self & Discover What You Want">
 How to Stop Playing Mind Games While Dating — Practical Tips for Honest Relationships">
How to Stop Playing Mind Games While Dating — Practical Tips for Honest Relationships">
 What Determines Sexual Attraction Exactly — Science, Psychology & Key Factors">
What Determines Sexual Attraction Exactly — Science, Psychology & Key Factors">
 What Is Emotional Lability? Causes, Symptoms & Treatment">
What Is Emotional Lability? Causes, Symptoms & Treatment">
 Happy Hormones – The Endocrine System and Brain Connection for Better Mood">
Happy Hormones – The Endocrine System and Brain Connection for Better Mood">
 How Many Types of Love Are There? 9 Types Explained">
How Many Types of Love Are There? 9 Types Explained">